Coagulation and fibrinolysis are vital processes that maintain the balance between blood clot formation and breakdown, preventing excessive bleeding or thrombosis. Disruptions in this equilibrium can lead to serious conditions such as deep vein thrombosis or hemorrhagic disorders. Explore the full article to understand how these mechanisms work together to protect your circulatory health.
Table of Comparison
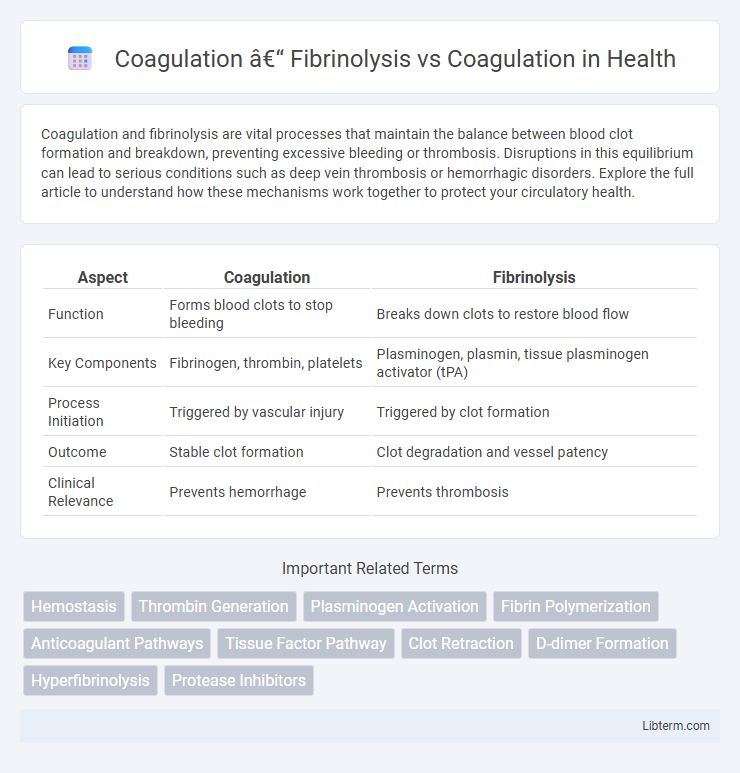
| Aspect | Coagulation | Fibrinolysis |
|---|---|---|
| Function | Forms blood clots to stop bleeding | Breaks down clots to restore blood flow |
| Key Components | Fibrinogen, thrombin, platelets | Plasminogen, plasmin, tissue plasminogen activator (tPA) |
| Process Initiation | Triggered by vascular injury | Triggered by clot formation |
| Outcome | Stable clot formation | Clot degradation and vessel patency |
| Clinical Relevance | Prevents hemorrhage | Prevents thrombosis |
Overview of Hemostasis: Coagulation and Fibrinolysis
Hemostasis is a dynamic balance between coagulation and fibrinolysis, crucial for maintaining vascular integrity after injury. Coagulation involves a cascade of enzymatic reactions that lead to the formation of a stable fibrin clot, preventing excessive bleeding. Fibrinolysis counteracts clot formation by enzymatically degrading fibrin through plasmin activity, ensuring timely clot removal and vascular patency.
Key Components of the Coagulation Cascade
The coagulation cascade involves a sequence of enzymatic reactions primarily driven by clotting factors such as Factor VII, IX, X, and prothrombin, culminating in the conversion of fibrinogen to fibrin to form a stable blood clot. Key components include tissue factor (TF), which initiates the extrinsic pathway, alongside intrinsic pathway factors and calcium ions (Factor IV) that facilitate complex formation and amplification. Fibrinolysis, in contrast, is regulated by enzymes like plasmin, which degrades fibrin, balancing clot formation to maintain vascular patency and prevent thrombosis.
Initiation and Progression of Fibrinolysis
Coagulation initiates through tissue factor exposure, activating the extrinsic pathway, leading to thrombin generation and fibrin clot formation, whereas fibrinolysis begins with plasminogen activation by tissue plasminogen activator (tPA) or urokinase, promoting fibrin degradation. During progression, coagulation amplifies via intrinsic and extrinsic pathways creating a stable fibrin mesh, while fibrinolysis escalates through plasmin activity breaking down fibrin into fibrin degradation products, restoring vascular patency. The balance between these processes is tightly regulated by inhibitors like plasminogen activator inhibitor-1 (PAI-1) and a2-antiplasmin, ensuring controlled clot dissolution without excessive bleeding.
Coagulation: Purpose, Triggers, and Mechanisms
Coagulation is the physiological process that stops bleeding by forming a stable blood clot through a complex cascade of enzymatic reactions involving clotting factors like fibrinogen and thrombin. Its primary purpose is to prevent excessive blood loss following vascular injury, triggered by endothelial damage, exposure of subendothelial collagen, and platelet activation. The coagulation mechanism proceeds via intrinsic and extrinsic pathways converging on the common pathway, culminating in fibrin mesh formation that stabilizes the platelet plug.
Fibrinolysis: Role in Clot Breakdown
Fibrinolysis plays a crucial role in clot breakdown by enzymatically degrading fibrin, the primary structural component of blood clots, through the activation of plasminogen to plasmin. This process ensures the removal of unnecessary clots, maintaining vascular patency and preventing thrombosis-related complications such as stroke or myocardial infarction. Imbalances between coagulation and fibrinolysis can lead to either excessive bleeding or pathological clot formation, highlighting fibrinolysis as a key target in therapeutic interventions for thrombotic diseases.
Major Differences Between Coagulation and Fibrinolysis
Coagulation is the biological process involving the transformation of blood from a liquid to a gel, primarily through the activation of clotting factors leading to fibrin mesh formation that stops bleeding. Fibrinolysis is the enzymatic breakdown of the fibrin clot, mainly mediated by plasmin, which restores normal blood flow and prevents thrombus propagation. The major differences lie in their functions: coagulation promotes clot formation to prevent hemorrhage, while fibrinolysis degrades clots to maintain vascular patency and tissue repair.
Regulatory Factors Controlling Coagulation and Fibrinolysis
Regulatory factors controlling coagulation and fibrinolysis maintain hemostatic balance by modulating enzyme activities and inhibitor concentrations, including antithrombin, protein C, and tissue factor pathway inhibitor for coagulation, and plasminogen activators as well as plasmin inhibitors such as a2-antiplasmin in fibrinolysis. Precise control is achieved through feedback mechanisms and localized activation at injury sites, preventing excessive clot formation or degradation. Dysregulation of these factors often leads to pathological conditions like thrombosis or hemorrhage.
Clinical Disorders Linked to Coagulation and Fibrinolysis Imbalance
Imbalances in coagulation and fibrinolysis disrupt hemostatic equilibrium, leading to clinical disorders such as disseminated intravascular coagulation (DIC), venous thromboembolism (VTE), and bleeding diatheses. Excessive coagulation activation results in thrombosis and organ ischemia, while impaired fibrinolysis hinders clot breakdown, exacerbating vascular occlusion. Conversely, hyperactive fibrinolysis causes uncontrolled bleeding by accelerating clot degradation, highlighting the critical role of regulated coagulation-fibrinolysis interplay in maintaining vascular health.
Diagnostic Approaches: Evaluating Coagulation and Fibrinolytic Activity
Diagnostic approaches for evaluating coagulation and fibrinolytic activity include assays such as prothrombin time (PT), activated partial thromboplastin time (aPTT), thrombin time (TT), and D-dimer tests, which collectively assess clot formation and breakdown. Viscoelastic tests like thromboelastography (TEG) and rotational thromboelastometry (ROTEM) provide dynamic, real-time analysis of clot kinetics, including fibrinolysis. Measuring specific biomarkers, such as plasminogen, tissue plasminogen activator (tPA), and plasmin inhibitor levels, enhances the accuracy of fibrinolytic activity assessment in clinical settings.
Therapeutic Implications: Targeting Coagulation vs Fibrinolysis
Targeting coagulation pathways primarily involves the use of anticoagulants such as heparin, warfarin, and direct oral anticoagulants (DOACs) to prevent thrombus formation in conditions like deep vein thrombosis and atrial fibrillation. Therapeutic strategies aimed at fibrinolysis focus on enhancing clot breakdown through agents like tissue plasminogen activator (tPA), which are critical in the management of acute ischemic stroke and pulmonary embolism. Optimizing the balance between coagulation inhibition and fibrinolytic activation remains essential for reducing thrombotic risk while minimizing bleeding complications in clinical practice.
Coagulation – Fibrinolysis Infographic
 libterm.com
libterm.com