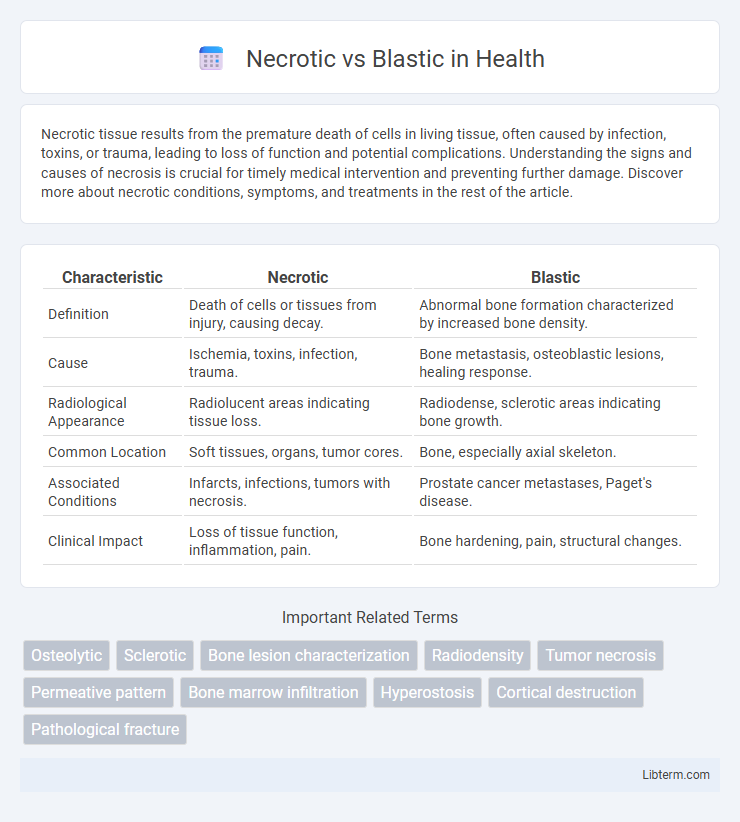
Necrotic tissue results from the premature death of cells in living tissue, often caused by infection, toxins, or trauma, leading to loss of function and potential complications. Understanding the signs and causes of necrosis is crucial for timely medical intervention and preventing further damage. Discover more about necrotic conditions, symptoms, and treatments in the rest of the article.
Table of Comparison
| Characteristic | Necrotic | Blastic |
|---|---|---|
| Definition | Death of cells or tissues from injury, causing decay. | Abnormal bone formation characterized by increased bone density. |
| Cause | Ischemia, toxins, infection, trauma. | Bone metastasis, osteoblastic lesions, healing response. |
| Radiological Appearance | Radiolucent areas indicating tissue loss. | Radiodense, sclerotic areas indicating bone growth. |
| Common Location | Soft tissues, organs, tumor cores. | Bone, especially axial skeleton. |
| Associated Conditions | Infarcts, infections, tumors with necrosis. | Prostate cancer metastases, Paget's disease. |
| Clinical Impact | Loss of tissue function, inflammation, pain. | Bone hardening, pain, structural changes. |
Understanding Necrotic and Blastic Lesions
Necrotic lesions are characterized by tissue death resulting from factors like infection, ischemia, or trauma, leading to loss of cellular structure and function. Blastic lesions involve abnormal bone formation or increased osteoblastic activity, commonly seen in conditions such as prostate cancer metastases or osteosclerosis. Distinguishing between necrotic and blastic lesions is crucial for accurate diagnosis and targeted treatment, using imaging techniques like MRI, CT scans, and bone scans to assess their structural and metabolic differences.
Key Differences Between Necrotic and Blastic Processes
Necrotic processes involve the uncontrolled death of cells resulting in tissue damage, inflammation, and loss of function, commonly seen in conditions like infarction or infection. Blastic processes, in contrast, refer to the formation of new, immature cells, often related to rapid cell proliferation seen in cancers such as acute myeloid leukemia or blastic tumors. The key difference lies in necrosis causing tissue destruction, whereas blastic activity signifies abnormal cell growth and proliferation.
Causes of Necrotic Lesions
Necrotic lesions primarily result from ischemia, infection, toxins, or immune-mediated damage leading to tissue death and cellular breakdown. In contrast, blastic lesions are characterized by increased osteoblastic activity, often due to metastatic cancer or benign bone-forming processes. Understanding the underlying cause of necrosis involves evaluating factors such as vascular occlusion, bacterial invasion, or exposure to cytotoxic agents that disrupt normal cellular function.
Common Origins of Blastic Lesions
Blastic lesions commonly originate from metastatic prostate, breast, and lung cancers, which stimulate abnormal bone formation visible as sclerotic areas on imaging. These lesions result from increased osteoblastic activity leading to dense, hardened bone structures, often associated with specific malignancies such as prostate adenocarcinoma. Differentiation from necrotic lesions, characterized by bone destruction and lytic appearance, is critical for accurate diagnosis and treatment planning.
Clinical Presentation: Necrotic vs. Blastic
Necrotic lesions typically present with tissue death characterized by blackened, foul-smelling areas often accompanied by pain and signs of infection, whereas blastic lesions manifest as abnormal bone growths resulting in localized swelling and increased bone density observable on imaging. Clinically, necrotic tissue may show ulceration and delayed healing, contrasting with the firm, sclerotic texture noted in blastic bone changes. The distinct presentation aids in differential diagnosis, guiding targeted treatment strategies for necrotic versus blastic conditions.
Diagnostic Imaging: Spotting the Differences
Necrotic lesions typically appear as areas of low density with central lucency on CT scans or hypointense regions on T1-weighted MRI, indicating tissue death. Blastic lesions, in contrast, present as sclerotic or high-density zones on imaging, reflecting increased bone formation and mineralization. Differentiating these patterns through diagnostic imaging aids clinicians in accurately identifying underlying pathologies such as metastatic cancers or infections.
Histopathological Features: Necrotic vs. Blastic
Necrotic lesions display extensive tissue death characterized by cellular debris, loss of nuclear detail, and eosinophilic cytoplasm under histopathological examination. Blastic lesions show increased osteoblastic activity with dense, sclerotic bone formation and prominent osteoid seams. The distinct histopathological features assist in differentiating necrotic tissue, marked by hypoxia and cell death, from blastic tissue, associated with new bone synthesis and repair.
Treatment Strategies for Necrotic vs. Blastic Lesions
Treatment strategies for necrotic lesions often involve aggressive debridement, antibiotics, and supportive care to manage infection and promote tissue regeneration, whereas blastic lesions require targeted therapies such as bisphosphonates or radiopharmaceuticals to control abnormal bone growth and reduce sclerosis. Management of necrotic bone focuses on restoring blood supply and preventing further necrosis, while blastic lesion treatment targets the underlying pathology of increased osteoblastic activity, often seen in metastatic bone disease. Tailored approaches based on lesion type improve patient outcomes by addressing distinct pathological mechanisms in necrotic versus blastic bone lesions.
Prognosis and Patient Outcomes
Necrotic lesions typically indicate tissue death caused by insufficient blood supply or infection, often associated with poorer prognosis due to increased risk of complications such as infection and delayed healing. Blastic lesions represent abnormal new bone formation usually seen in metastatic prostate cancer and generally correlate with a more favorable prognosis compared to necrotic lesions, as these tend to indicate a slower disease progression. Patient outcomes differ significantly, with blastic lesions often responding better to treatment and exhibiting longer survival rates, whereas necrotic lesions may require more aggressive management to prevent adverse effects.
Future Perspectives in Necrotic and Blastic Research
Future perspectives in necrotic and blastic research emphasize the development of targeted therapies that address the distinct molecular pathways involved in tissue degradation and abnormal bone formation. Advances in imaging modalities and biomarker identification are expected to enhance early diagnosis and treatment monitoring for necrotic lesions and blastic bone metastases. Emerging studies on genetic and epigenetic factors promise personalized medicine approaches to improve patient outcomes in managing necrotic and blastic conditions.
Necrotic Infographic
 libterm.com
libterm.com