Placebo and active treatment serve distinct roles in clinical trials, with placebos designed to mimic the appearance of real medications without containing active ingredients. Understanding the differences in their effects helps researchers determine the true efficacy of new drugs and treatments. Explore the rest of this article to learn how placebos impact your treatment outcomes and clinical research.
Table of Comparison
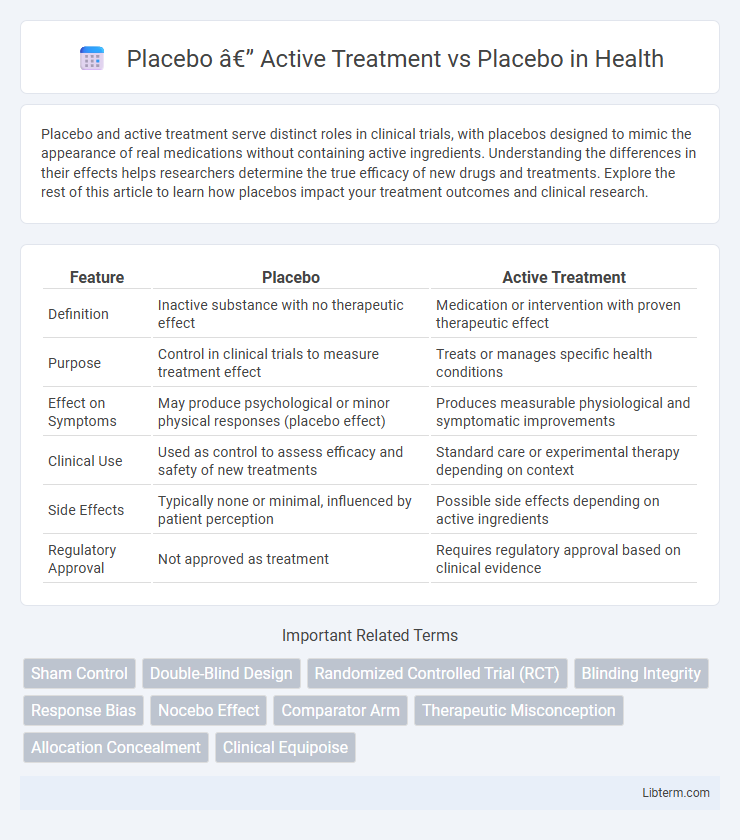
| Feature | Placebo | Active Treatment |
|---|---|---|
| Definition | Inactive substance with no therapeutic effect | Medication or intervention with proven therapeutic effect |
| Purpose | Control in clinical trials to measure treatment effect | Treats or manages specific health conditions |
| Effect on Symptoms | May produce psychological or minor physical responses (placebo effect) | Produces measurable physiological and symptomatic improvements |
| Clinical Use | Used as control to assess efficacy and safety of new treatments | Standard care or experimental therapy depending on context |
| Side Effects | Typically none or minimal, influenced by patient perception | Possible side effects depending on active ingredients |
| Regulatory Approval | Not approved as treatment | Requires regulatory approval based on clinical evidence |
Introduction to Placebo and Active Treatment
Placebo refers to a substance or treatment with no therapeutic effect, commonly used as a control in clinical trials to assess the efficacy of active treatments. Active treatment involves administering a drug, therapy, or intervention designed to produce a specific physiological or psychological effect on a patient. Comparing active treatment versus placebo helps determine the true effectiveness of a medical intervention by isolating its impact beyond patients' expectations or natural progression of disease.
Defining the Placebo Effect
The placebo effect refers to the measurable, observable, or felt improvement in health not attributable to the active ingredients of a treatment but rather to the patient's expectations and beliefs. In clinical trials comparing active treatment vs placebo, this effect underscores the psychological and physiological responses triggered by receiving a sham intervention. Understanding the placebo effect is crucial for accurately interpreting treatment efficacy and isolating true pharmacological benefits in therapeutic studies.
Mechanisms Behind Placebo Responses
Placebo responses arise from complex neurobiological mechanisms involving brain regions such as the prefrontal cortex, anterior cingulate cortex, and neurotransmitters like dopamine and endorphins. These mechanisms activate endogenous pain relief and emotional regulatory pathways, leading to measurable physiological and psychological effects despite the absence of active treatment. Understanding these processes enhances clinical trial design and optimizes therapeutic strategies by leveraging patient expectations and conditioning.
Distinguishing Active Treatment from Placebo
Distinguishing active treatment from placebo involves identifying physiological or psychological effects directly caused by the active drug rather than by patient expectations or natural disease progression. Biomarkers, objective clinical outcomes, and double-blind randomized controlled trials are key methods used to separate true drug efficacy from placebo responses. Understanding this differentiation is crucial for evaluating drug effectiveness and ensuring accurate clinical decision-making.
Clinical Trials: Placebo-Controlled vs Active-Controlled
Clinical trials that compare active treatment versus placebo focus on assessing the efficacy and safety of new interventions by using placebo-controlled or active-controlled designs. Placebo-controlled trials administer an inert substance to the control group, providing a baseline to measure the actual drug's effect, which is essential for establishing efficacy in conditions with subjective outcomes. Active-controlled trials, by using an existing approved treatment instead of a placebo, are vital for determining whether a new drug is at least as effective or safer than current standard therapies, especially when withholding treatment is unethical.
Ethical Considerations of Placebo Use
The ethical considerations of using placebo in clinical trials center on balancing scientific validity with patient welfare, ensuring informed consent, and minimizing harm by providing the best available care alongside placebo administration. Placebo use is ethically justified primarily when no proven effective treatment exists or when withholding treatment does not pose serious harm to participants. Institutional review boards and guidelines such as the Declaration of Helsinki emphasize transparency, participant autonomy, and rigorous risk-benefit assessments to uphold ethical standards in placebo-controlled studies.
Measuring Treatment Outcomes: Placebo vs Active
Measuring treatment outcomes in placebo versus active treatment trials involves analyzing changes in patient-reported symptoms, clinical assessments, and biomarker levels to determine efficacy. Active treatments typically demonstrate statistically significant improvements over placebo in controlled randomized trials, reflecting true pharmacological effects. Placebo responses highlight the psychological and neurobiological influence on perceived symptom relief, underscoring the necessity for rigorous blinding and objective measurement criteria.
Impact of Placebo in Different Medical Conditions
The impact of placebo varies significantly across medical conditions, demonstrating strong effects in pain management, depression, and irritable bowel syndrome due to patients' expectations and brain chemistry changes. In neurological disorders and cardiovascular diseases, the placebo effect tends to be less pronounced but can still influence subjective symptoms and treatment adherence. Understanding placebo mechanisms enhances clinical trial design and informs healthcare providers on patient outcomes beyond pharmacological interventions.
Limitations of Placebo-Controlled Studies
Placebo-controlled studies often face limitations such as the difficulty in maintaining effective blinding, which can lead to biased patient or investigator expectations affecting outcomes. Ethical concerns arise when withholding active treatment, especially in serious or life-threatening conditions, limiting study design feasibility. Variability in placebo responses across populations and conditions complicates result interpretation and can obscure the true efficacy of the active treatment.
Future Directions in Placebo Research
Future directions in placebo research emphasize the integration of neuroimaging and personalized medicine to enhance the understanding of placebo responses in active treatment comparisons. Advances in genetic profiling and machine learning algorithms are being explored to predict individual placebo responsiveness, aiming to refine clinical trial designs. Ongoing studies focus on leveraging placebo mechanisms to improve therapeutic outcomes and minimize adverse effects across various medical conditions.
Placebo — Active Treatment Infographic
 libterm.com
libterm.com