Infections occur when harmful microorganisms such as bacteria, viruses, or fungi invade the body, triggering an immune response and causing symptoms that range from mild to severe. Early identification and proper treatment are essential to prevent complications and promote faster recovery. Explore the full article to learn how you can recognize infection signs and protect your health effectively.
Table of Comparison
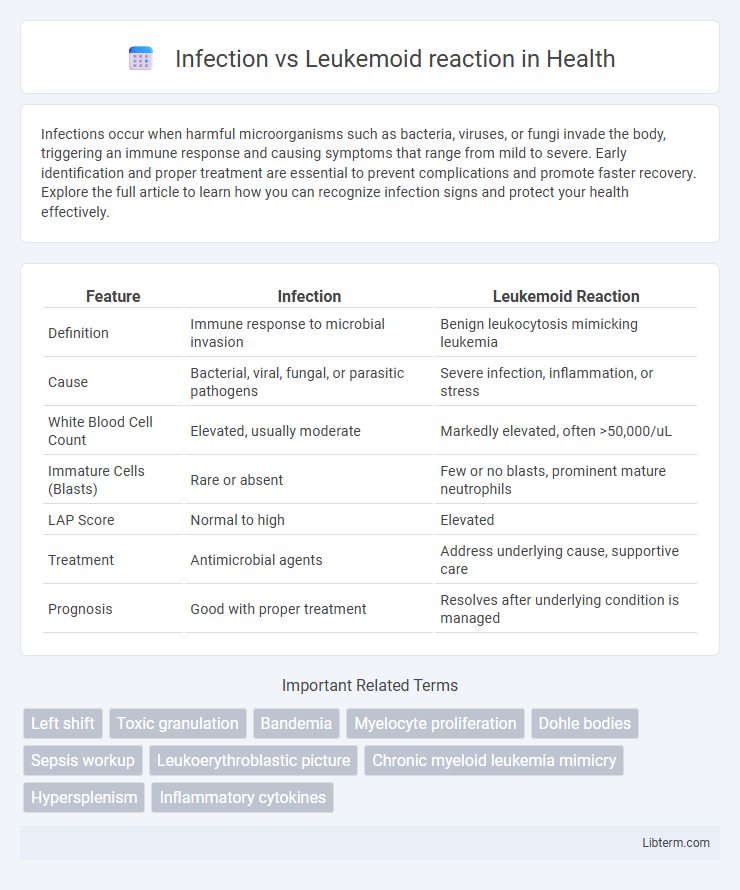
| Feature | Infection | Leukemoid Reaction |
|---|---|---|
| Definition | Immune response to microbial invasion | Benign leukocytosis mimicking leukemia |
| Cause | Bacterial, viral, fungal, or parasitic pathogens | Severe infection, inflammation, or stress |
| White Blood Cell Count | Elevated, usually moderate | Markedly elevated, often >50,000/uL |
| Immature Cells (Blasts) | Rare or absent | Few or no blasts, prominent mature neutrophils |
| LAP Score | Normal to high | Elevated |
| Treatment | Antimicrobial agents | Address underlying cause, supportive care |
| Prognosis | Good with proper treatment | Resolves after underlying condition is managed |
Introduction: Understanding Infection and Leukemoid Reaction
Infection triggers an immune response characterized by elevated white blood cell counts to combat pathogens, while leukemoid reaction mimics leukemia with marked leukocytosis unrelated to malignant proliferation. Differentiating between infection-induced leukocytosis and leukemoid reaction requires careful analysis of clinical presentation, laboratory markers such as leukocyte alkaline phosphatase (LAP) score, and underlying causes like severe infections or stress. Accurate diagnosis is essential to avoid confusion with hematologic malignancies and to guide appropriate treatment strategies.
Definition of Infection
Infection is the invasion and multiplication of pathogenic microorganisms such as bacteria, viruses, fungi, or parasites within the body, leading to tissue damage and immune response activation. It commonly results in systemic symptoms like fever, elevated white blood cell count, and localized inflammation depending on the site of pathogen entry. Differentiating infection from leukemoid reaction requires clinical evaluation and laboratory tests, as leukemoid reactions mimic leukemia with marked leukocytosis but are reactive processes to stress or infection rather than true malignancy.
Definition of Leukemoid Reaction
Leukemoid reaction is defined as a transient, benign increase in white blood cell count that mimics leukemia but results from infection, inflammation, or other stressors. Unlike leukemia, leukemoid reaction does not involve malignant proliferation of hematopoietic cells and is characterized by a marked elevation of mature neutrophils with toxic granulation. Distinguishing leukemoid reaction from infection-induced leukocytosis relies on clinical context, peripheral smear analysis, and bone marrow examination.
Etiology: Causes of Infection vs Leukemoid Reaction
Infections are primarily caused by pathogenic microorganisms such as bacteria, viruses, fungi, and parasites that invade the body, triggering an immune response. Leukemoid reactions occur due to severe stress or stimuli like infections, certain drugs, malignancies, or hemorrhage, leading to an exaggerated white blood cell production resembling leukemia. While infections directly result from microbial invasion, leukemoid reactions represent a reactive, non-neoplastic increase in leukocytes often secondary to systemic insults.
Clinical Manifestations and Key Differences
Infections often present with fever, localized symptoms such as redness or swelling, and elevated white blood cell (WBC) counts predominantly neutrophilia, whereas leukemoid reactions exhibit extreme leukocytosis, often exceeding 50,000 WBCs/uL with a left shift including immature granulocytes like myelocytes and metamyelocytes. Unlike leukemia, leukemoid reactions lack blasts in the peripheral smear and typically resolve after treating the underlying cause, often reflected by a high leukocyte alkaline phosphatase (LAP) score. Clinical manifestations of leukemoid reactions may mimic leukemia but are usually distinguishable by the absence of clonal proliferation and bone marrow infiltration seen in leukemia.
Laboratory Findings: Distinguishing Parameters
Infection and leukemoid reaction can both present with elevated white blood cell counts, but laboratory findings reveal key distinctions. Leukemoid reactions often exhibit a marked increase in leukocyte alkaline phosphatase (LAP) score, whereas infections typically show low or normal LAP levels. The presence of immature myeloid cells and a left shift is common in both, but leukemoid reactions lack the clonal markers found in chronic myeloid leukemia, aiding differential diagnosis through cytogenetic studies.
Pathophysiology: Mechanisms Behind Infection and Leukemoid Reaction
Infections trigger leukemoid reactions through the release of inflammatory cytokines such as interleukin-1 (IL-1) and tumor necrosis factor-alpha (TNF-a), stimulating bone marrow to produce a marked leukocytosis resembling leukemia. Leukemoid reactions are characterized by exaggerated neutrophil proliferation and a left shift in the peripheral blood, primarily driven by granulocyte colony-stimulating factor (G-CSF) during severe infections or stress. Unlike malignancies, this mechanism is a reactive process, where bone marrow retains normal maturation cues despite the high white blood cell count.
Diagnostic Approaches and Differential Diagnosis
Diagnostic approaches distinguishing infection from leukemoid reaction emphasize comprehensive blood analysis, including peripheral smear examination and leukocyte alkaline phosphatase (LAP) score assessment, where leukemoid reaction typically presents with elevated LAP. Microbiological cultures and inflammatory markers such as C-reactive protein (CRP) and procalcitonin assist in confirming infections, particularly bacterial sepsis, which rarely elevates LAP scores. Differential diagnosis requires careful evaluation of clinical context, history of infection or malignancy, and exclusion of chronic myelogenous leukemia (CML) using cytogenetic or molecular tests like BCR-ABL1 gene rearrangement analysis.
Treatment Strategies for Infection versus Leukemoid Reaction
Treatment for infection focuses on identifying and eradicating the underlying pathogen using targeted antibiotics, antivirals, or antifungals based on culture and sensitivity results, along with supportive care to manage symptoms and prevent complications. Leukemoid reaction, often a response to severe infection or stress, necessitates addressing the primary cause such as infection or inflammation while avoiding unnecessary chemotherapy used for leukemia. Close monitoring of white blood cell counts and clinical status guides therapy adjustments and distinguishes the benign leukemoid response from malignant conditions.
Prognosis and Clinical Outcomes
Infection-induced leukemoid reactions generally have a favorable prognosis as they resolve with appropriate antimicrobial treatment, contrasting with the more variable outcomes of leukemoid reactions linked to malignancies or severe systemic diseases. Clinical outcomes depend on the underlying cause, where infectious etiologies often result in rapid normalization of white blood cell counts once the infection is controlled. Persistent leukocytosis with poor clinical improvement may indicate a need for further evaluation to rule out hematologic disorders or malignancies impacting prognosis.
Infection Infographic
 libterm.com
libterm.com