Pancreatitis is an inflammation of the pancreas that can cause severe abdominal pain and digestive issues. It often results from gallstones, excessive alcohol consumption, or certain medications, leading to symptoms like nausea, vomiting, and fever. Discover how to recognize the signs, manage symptoms, and explore effective treatments by reading the rest of the article.
Table of Comparison
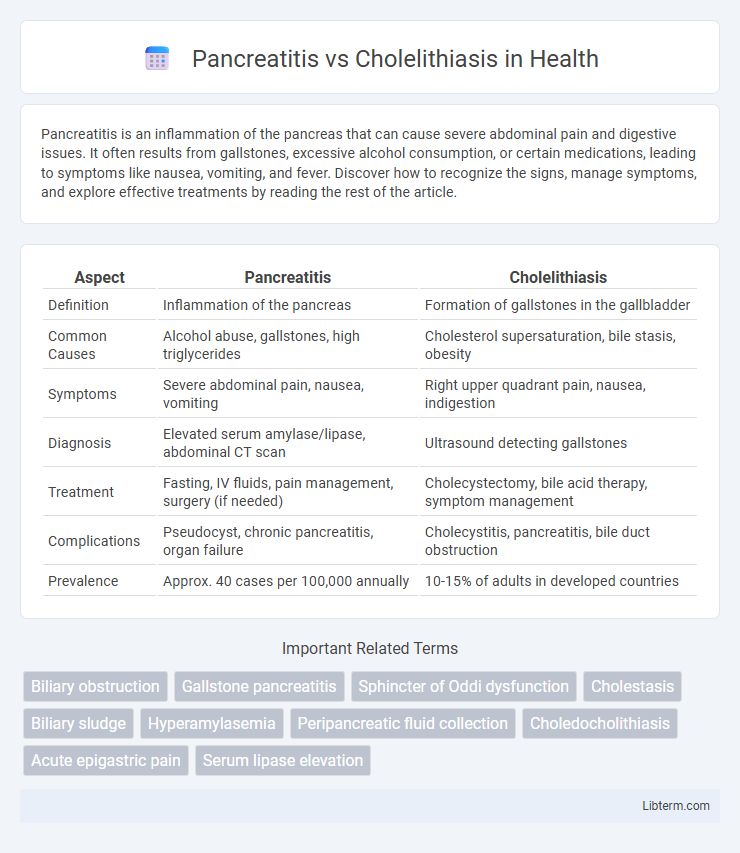
| Aspect | Pancreatitis | Cholelithiasis |
|---|---|---|
| Definition | Inflammation of the pancreas | Formation of gallstones in the gallbladder |
| Common Causes | Alcohol abuse, gallstones, high triglycerides | Cholesterol supersaturation, bile stasis, obesity |
| Symptoms | Severe abdominal pain, nausea, vomiting | Right upper quadrant pain, nausea, indigestion |
| Diagnosis | Elevated serum amylase/lipase, abdominal CT scan | Ultrasound detecting gallstones |
| Treatment | Fasting, IV fluids, pain management, surgery (if needed) | Cholecystectomy, bile acid therapy, symptom management |
| Complications | Pseudocyst, chronic pancreatitis, organ failure | Cholecystitis, pancreatitis, bile duct obstruction |
| Prevalence | Approx. 40 cases per 100,000 annually | 10-15% of adults in developed countries |
Understanding Pancreatitis: Definition and Causes
Pancreatitis is the inflammation of the pancreas characterized by abdominal pain and digestive enzyme dysfunction, often triggered by gallstones, excessive alcohol consumption, or genetic factors. Cholelithiasis, the presence of gallstones in the gallbladder, frequently causes pancreatitis by obstructing the pancreatic duct, leading to enzyme activation within the pancreas itself. Understanding the pathophysiology of pancreatitis requires recognizing the role of gallstone-induced bile duct obstruction and other etiologies like triglyceride-induced damage or autoimmune conditions.
Cholelithiasis: What Are Gallstones?
Cholelithiasis refers to the formation of gallstones, which are hardened deposits primarily composed of cholesterol, bilirubin, and calcium salts that develop in the gallbladder. Gallstones can block bile ducts, leading to pain, inflammation, and digestive issues, distinguishing the condition from pancreatitis, which is inflammation of the pancreas often caused by gallstones obstructing the pancreatic duct. Diagnosis and treatment of cholelithiasis involve imaging techniques like ultrasound and may require dietary management or surgical intervention such as cholecystectomy.
Key Differences Between Pancreatitis and Cholelithiasis
Pancreatitis involves inflammation of the pancreas, often caused by gallstones blocking the pancreatic duct or excessive alcohol use, while cholelithiasis refers specifically to the presence of gallstones in the gallbladder without inflammation. Clinically, pancreatitis presents with severe upper abdominal pain, elevated pancreatic enzymes (amylase and lipase), and systemic symptoms, whereas cholelithiasis may be asymptomatic or cause biliary colic with intermittent right upper quadrant pain. Diagnostic imaging for pancreatitis includes abdominal CT or MRI to assess pancreatic inflammation, whereas ultrasonography is the preferred method to detect gallstones in cholelithiasis.
Risk Factors for Developing Pancreatitis and Cholelithiasis
Risk factors for developing pancreatitis include chronic alcohol consumption, gallstones, hypertriglyceridemia, smoking, and certain medications such as corticosteroids or diuretics. Cholelithiasis risk factors encompass obesity, female sex, age over 40, rapid weight loss, pregnancy, and a family history of gallstones. Both conditions share gallstones as a common risk factor, linking biliary obstruction to the onset of pancreatitis.
Common Symptoms: How They Overlap and Differ
Pancreatitis and cholelithiasis both commonly present with upper abdominal pain, often radiating to the back, along with nausea and vomiting, making initial clinical differentiation challenging. Pancreatitis typically causes persistent, severe epigastric pain aggravated by eating, whereas cholelithiasis often triggers episodic, colicky right upper quadrant pain associated with fatty meals. Elevated serum amylase and lipase levels are characteristic of pancreatitis, while cholelithiasis may show liver function test abnormalities and ultrasound evidence of gallstones.
Diagnostic Approaches for Pancreatitis vs Cholelithiasis
Diagnostic approaches for pancreatitis primarily include elevated serum amylase and lipase levels, abdominal ultrasound, and contrast-enhanced CT scans to assess pancreatic inflammation and complications. Cholelithiasis diagnosis relies on abdominal ultrasound to detect gallstones, with hepatobiliary iminodiacetic acid (HIDA) scans or MRCP used to evaluate bile duct obstruction. Both conditions require liver function tests to differentiate pancreatic involvement from biliary pathology accurately.
Treatment Options for Pancreatitis
Treatment options for pancreatitis primarily involve supportive care, including fluid resuscitation, pain management, and nutritional support, often through fasting and intravenous fluids to rest the pancreas. In severe cases, interventions such as endoscopic retrograde cholangiopancreatography (ERCP) may be required to remove bile duct obstructions if gallstones cause pancreatitis, while surgical options are considered for complications like necrosis or infection. Addressing the underlying causes, such as gallstone removal or managing alcohol use, is essential to prevent recurrent episodes and promote recovery.
Management and Treatment of Cholelithiasis
Cholelithiasis management primarily involves the removal of gallstones through laparoscopic cholecystectomy, which is the gold standard treatment to prevent complications such as pancreatitis. Medical management with ursodeoxycholic acid may be considered for patients who are poor surgical candidates or prefer non-surgical treatment, although its efficacy is limited to cholesterol-based stones. Pain control, hydration, and treating any associated infections are essential supportive measures before and after definitive treatment.
Potential Complications: Comparing Both Conditions
Pancreatitis can lead to severe complications such as pancreatic necrosis, abscess formation, and systemic inflammatory response syndrome (SIRS), which may result in multi-organ failure. Cholelithiasis often causes complications including acute cholecystitis, choledocholithiasis, and gallbladder perforation, increasing the risk of biliary sepsis. Both conditions share the potential for biliary obstruction and infections but differ in the severity of systemic inflammatory responses and long-term organ damage risks.
Prevention Strategies for Pancreatitis and Cholelithiasis
Effective prevention strategies for pancreatitis include maintaining a low-fat diet, limiting alcohol consumption, and managing triglyceride levels to reduce inflammation in the pancreas. In cholelithiasis, preventing gallstone formation involves weight management through regular exercise, a high-fiber diet, and avoiding rapid weight loss that can disrupt bile salt balance. Regular medical check-ups can help identify risk factors early, facilitating timely interventions to prevent complications associated with both conditions.
Pancreatitis Infographic
 libterm.com
libterm.com