Cholestasis occurs when bile flow from the liver is reduced or blocked, leading to accumulation of bile acids in the liver and bloodstream. This condition can cause symptoms such as itching, jaundice, and digestive issues, and may result from liver diseases, bile duct obstructions, or certain medications. Discover more about the causes, symptoms, and treatment options to protect your liver health in the rest of this article.
Table of Comparison
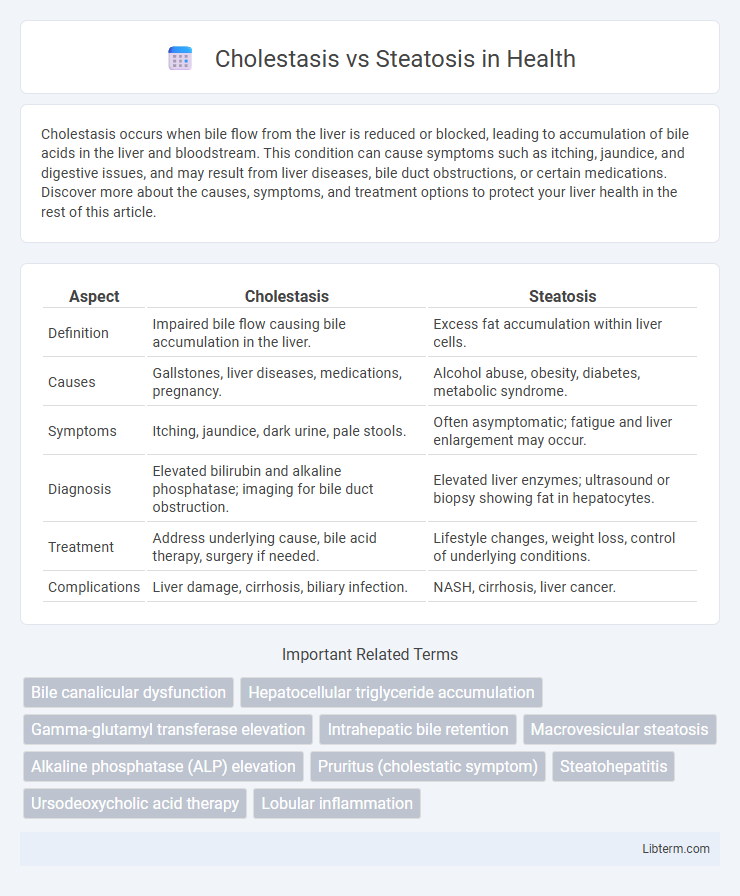
| Aspect | Cholestasis | Steatosis |
|---|---|---|
| Definition | Impaired bile flow causing bile accumulation in the liver. | Excess fat accumulation within liver cells. |
| Causes | Gallstones, liver diseases, medications, pregnancy. | Alcohol abuse, obesity, diabetes, metabolic syndrome. |
| Symptoms | Itching, jaundice, dark urine, pale stools. | Often asymptomatic; fatigue and liver enlargement may occur. |
| Diagnosis | Elevated bilirubin and alkaline phosphatase; imaging for bile duct obstruction. | Elevated liver enzymes; ultrasound or biopsy showing fat in hepatocytes. |
| Treatment | Address underlying cause, bile acid therapy, surgery if needed. | Lifestyle changes, weight loss, control of underlying conditions. |
| Complications | Liver damage, cirrhosis, biliary infection. | NASH, cirrhosis, liver cancer. |
Understanding Cholestasis: Definition and Causes
Cholestasis is a condition characterized by impaired bile flow from the liver to the duodenum, leading to the accumulation of bile acids and bilirubin in the liver and bloodstream. Common causes include intrahepatic factors such as liver diseases (e.g., primary biliary cholangitis, hepatitis) and extrahepatic obstructions like gallstones or tumors blocking the bile ducts. Understanding cholestasis involves recognizing these etiologies to differentiate it from steatosis, which refers to fatty liver accumulation without bile flow obstruction.
Defining Steatosis: Overview and Etiology
Steatosis, also known as fatty liver disease, is characterized by excessive accumulation of triglycerides in hepatocytes, leading to liver dysfunction. The etiology of steatosis includes metabolic factors such as obesity, type 2 diabetes, insulin resistance, alcohol consumption, and certain medications. Unlike cholestasis, which involves impaired bile flow, steatosis primarily results from disruptions in lipid metabolism and fat storage within liver cells.
Key Differences Between Cholestasis and Steatosis
Cholestasis involves impaired bile flow causing bile accumulation in the liver, characterized by elevated bilirubin and alkaline phosphatase levels, whereas steatosis is the accumulation of fat within hepatocytes, often linked to metabolic syndrome and elevated liver enzymes like ALT and AST. Cholestasis manifests clinically with jaundice, pruritus, and pale stools, while steatosis may remain asymptomatic or present with hepatomegaly and nonspecific symptoms. Diagnostic imaging and liver biopsy differentiate these conditions by detecting bile duct obstruction in cholestasis versus lipid accumulation in steatosis.
Clinical Manifestations of Cholestasis
Cholestasis presents clinically with pruritus, jaundice, dark urine, and pale stools due to impaired bile flow and accumulation of bile acids. Patients often experience fatigue and right upper quadrant pain, reflecting hepatocellular injury or biliary obstruction. Laboratory findings typically reveal elevated alkaline phosphatase, gamma-glutamyl transferase, and conjugated hyperbilirubinemia.
Symptoms and Signs of Steatosis
Steatosis, commonly known as fatty liver disease, often presents with symptoms like fatigue, abdominal discomfort, and hepatomegaly, sometimes accompanied by elevated liver enzymes in blood tests. In contrast, cholestasis is characterized by jaundice, pruritus, dark urine, and pale stools, resulting from impaired bile flow. Recognition of steatosis symptoms aids early diagnosis, preventing progression to steatohepatitis or cirrhosis.
Diagnostic Approaches: Cholestasis vs Steatosis
Diagnostic approaches for cholestasis primarily involve liver function tests showing elevated alkaline phosphatase and gamma-glutamyl transferase levels, along with imaging modalities like ultrasound, MRCP, or ERCP to identify bile duct obstruction. In contrast, steatosis diagnosis relies on imaging techniques such as ultrasonography, CT, and MRI demonstrating hepatic fat accumulation, with liver biopsy as the gold standard for confirming steatosis and assessing inflammation or fibrosis. Biomarkers for cholestasis include elevated conjugated bilirubin, whereas steatosis is generally associated with metabolic panels indicating insulin resistance or dyslipidemia.
Imaging and Laboratory Findings
Cholestasis typically presents with elevated alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT) levels, along with increased bilirubin on laboratory tests, while imaging such as ultrasound or MRCP reveals bile duct dilation or obstruction. Steatosis shows elevated liver enzymes, primarily alanine aminotransferase (ALT) and aspartate aminotransferase (AST), with imaging through ultrasound revealing increased echogenicity of the liver and MRI quantifying fat accumulation without bile duct abnormalities. Laboratory findings in steatosis often lack cholestatic markers, distinguishing it from cholestasis, which is characterized by impaired bile flow and associated biochemical profiles.
Pathophysiological Mechanisms: Comparing Both Conditions
Cholestasis involves impaired bile flow leading to accumulation of bile acids in hepatocytes, causing cellular toxicity and inflammation, primarily through disrupted bile salt export pumps and canalicular transporters. In contrast, steatosis is characterized by excessive triglyceride accumulation in hepatocytes due to imbalances in lipid metabolism, including increased fatty acid uptake, de novo lipogenesis, and impaired b-oxidation. Both conditions induce hepatocellular injury but via distinct mechanisms: cholestasis disrupts bile acid homeostasis affecting cellular membranes, whereas steatosis results from metabolic dysfunction and lipid overload within liver cells.
Treatment Strategies for Cholestasis and Steatosis
Treatment strategies for cholestasis primarily aim to relieve bile flow obstruction through medications like ursodeoxycholic acid, which improves bile secretion and reduces liver damage. In contrast, steatosis management focuses on lifestyle modifications such as weight loss, dietary changes, and controlling metabolic factors like diabetes and hyperlipidemia to reduce liver fat accumulation. Both conditions may require monitoring liver enzyme levels and addressing underlying causes to prevent progression to cirrhosis or liver failure.
Prognosis and Long-term Outcomes
Cholestasis, characterized by impaired bile flow, often leads to progressive liver damage and increased risk of fibrosis, cirrhosis, and liver failure if untreated, with prognosis depending on the underlying cause and timely intervention. Steatosis, or fatty liver disease, ranges from simple steatosis with a relatively benign course to steatohepatitis, which can progress to fibrosis and cirrhosis, strongly influenced by metabolic factors like obesity and diabetes. Long-term outcomes in both conditions improve significantly with early diagnosis, lifestyle modification, and management of associated risk factors.
Cholestasis Infographic
 libterm.com
libterm.com