Narcolepsy is a chronic neurological disorder characterized by excessive daytime sleepiness and sudden sleep attacks, often accompanied by cataplexy, which causes sudden muscle weakness triggered by strong emotions. Understanding the symptoms and treatment options can significantly improve your quality of life and help manage these disruptive episodes. Discover more about how to recognize and cope with narcolepsy and cataplexy in the rest of this article.
Table of Comparison
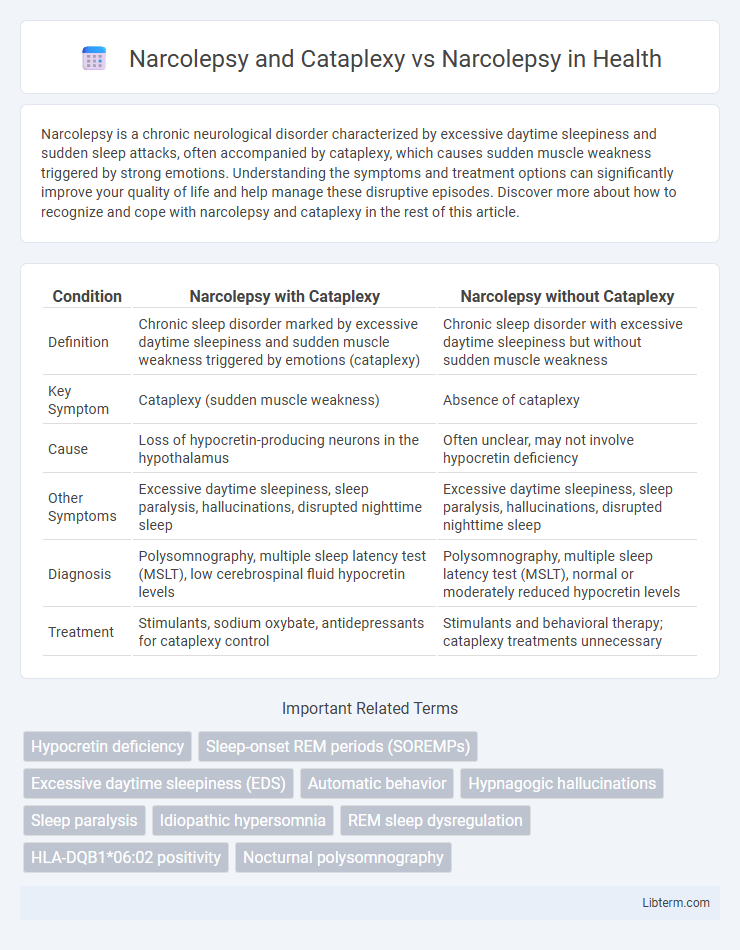
| Condition | Narcolepsy with Cataplexy | Narcolepsy without Cataplexy |
|---|---|---|
| Definition | Chronic sleep disorder marked by excessive daytime sleepiness and sudden muscle weakness triggered by emotions (cataplexy) | Chronic sleep disorder with excessive daytime sleepiness but without sudden muscle weakness |
| Key Symptom | Cataplexy (sudden muscle weakness) | Absence of cataplexy |
| Cause | Loss of hypocretin-producing neurons in the hypothalamus | Often unclear, may not involve hypocretin deficiency |
| Other Symptoms | Excessive daytime sleepiness, sleep paralysis, hallucinations, disrupted nighttime sleep | Excessive daytime sleepiness, sleep paralysis, hallucinations, disrupted nighttime sleep |
| Diagnosis | Polysomnography, multiple sleep latency test (MSLT), low cerebrospinal fluid hypocretin levels | Polysomnography, multiple sleep latency test (MSLT), normal or moderately reduced hypocretin levels |
| Treatment | Stimulants, sodium oxybate, antidepressants for cataplexy control | Stimulants and behavioral therapy; cataplexy treatments unnecessary |
Understanding Narcolepsy: Definition and Types
Narcolepsy is a chronic neurological disorder characterized by excessive daytime sleepiness and sudden muscle weakness, known as cataplexy, which occurs in about 70% of cases. There are two main types: Narcolepsy Type 1, which includes cataplexy and low hypocretin levels, and Narcolepsy Type 2, which lacks cataplexy and typically has normal hypocretin levels. Understanding these distinctions helps in accurate diagnosis and targeted treatment strategies for managing symptoms effectively.
What Is Cataplexy? Key Features Explained
Cataplexy is a sudden, brief episode of muscle weakness or paralysis triggered by strong emotions, and it is a key feature present in narcolepsy type 1 but absent in narcolepsy type 2. Characterized by symptoms such as slurred speech, drooping eyelids, or complete collapse while consciousness remains intact, cataplexy differentiates narcolepsy subtype diagnosis and guides targeted treatment strategies. Recognizing cataplexy's distinct role in narcolepsy enhances diagnostic accuracy and improves patient management through tailored therapies.
Narcolepsy With vs. Without Cataplexy: Core Differences
Narcolepsy with cataplexy is characterized by sudden, brief episodes of muscle weakness triggered by strong emotions, while narcolepsy without cataplexy lacks these muscle control disruptions but still involves excessive daytime sleepiness and sudden sleep attacks. The presence of cataplexy is linked to a loss of hypocretin-producing neurons in the hypothalamus, which distinguishes type 1 narcolepsy (with cataplexy) from type 2 narcolepsy (without cataplexy). Diagnostic criteria, treatment approaches, and prognosis may vary based on the presence or absence of cataplexy, making accurate classification essential for effective management.
Symptoms Exclusive to Narcolepsy With Cataplexy
Narcolepsy with cataplexy is distinguished by sudden, transient episodes of muscle weakness triggered by strong emotions, a symptom absent in narcolepsy without cataplexy. Excessive daytime sleepiness, hallucinations at sleep onset or upon waking, and sleep paralysis occur in both types, but cataplexy's hallmark is the episodic loss of muscle tone without loss of consciousness. The presence of cataplexy often correlates with hypocretin deficiency in the hypothalamus, setting it apart from narcolepsy without cataplexy which may not show this neurochemical imbalance.
Diagnostic Criteria for Narcolepsy and Cataplexy
Narcolepsy is diagnosed through a combination of clinical history, polysomnography (PSG), and Multiple Sleep Latency Test (MSLT), emphasizing excessive daytime sleepiness and rapid entry into REM sleep. Cataplexy, a sudden loss of muscle tone often triggered by emotions, is a key symptom distinguishing narcolepsy type 1, confirmed through clinical evaluation and the presence of hypocretin-1 deficiency in cerebrospinal fluid. The International Classification of Sleep Disorders (ICSD-3) criteria require documenting both excessive daytime sleepiness and either cataplexy or low hypocretin-1 levels for a narcolepsy with cataplexy diagnosis.
Narcolepsy Without Cataplexy: Signs and Challenges
Narcolepsy without cataplexy, known as narcolepsy type 2, presents with excessive daytime sleepiness and sudden sleep attacks but lacks the hallmark muscle weakness episodes characteristic of cataplexy. Patients often face diagnostic challenges due to overlapping symptoms with other sleep disorders, resulting in delayed treatment. Key signs include disrupted nighttime sleep, hallucinations at sleep onset or upon waking, and sleep paralysis, complicating daily functioning and reducing quality of life.
Causes and Risk Factors: Narcolepsy vs. Cataplexy
Narcolepsy is a neurological disorder primarily caused by the loss of hypocretin-producing neurons in the hypothalamus, which regulates wakefulness, while cataplexy is a sudden episode of muscle weakness triggered by strong emotions and occurs in approximately 70% of narcolepsy type 1 cases. Genetic predisposition, particularly the presence of the HLA-DQB1*06:02 allele, and autoimmune factors play significant roles in the development of narcolepsy, whereas cataplexy is specifically linked to the same autoimmune-induced hypocretin neuron loss. Environmental triggers such as infections or stress may contribute to the onset of narcolepsy but do not independently cause cataplexy, which is considered a symptom rather than a distinct condition.
Treatment Approaches for Both Conditions
Treatment approaches for narcolepsy and cataplexy primarily include stimulants like modafinil and armodafinil to combat excessive daytime sleepiness, while sodium oxybate is specifically effective in reducing cataplexy episodes and improving nighttime sleep. Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants, are also utilized to suppress cataplexy, hypnagogic hallucinations, and sleep paralysis. Comprehensive management often combines pharmacologic treatment with lifestyle adjustments, including scheduled naps and sleep hygiene optimization, to enhance overall symptom control and quality of life.
Living With Narcolepsy: Managing Daily Life
Living with narcolepsy requires careful management of symptoms like excessive daytime sleepiness and sudden muscle weakness known as cataplexy. Developing consistent sleep schedules, using prescribed stimulant medications, and incorporating scheduled naps improve alertness and reduce the impact on daily activities. Support from healthcare providers and educational resources helps individuals maintain productivity and safety despite the challenges of narcolepsy and cataplexy.
Narcolepsy and Cataplexy: Prognosis and Support
Narcolepsy with cataplexy typically presents with sudden muscle weakness triggered by strong emotions, distinguishing it from narcolepsy without cataplexy. The prognosis for narcolepsy with cataplexy involves managing symptoms through lifestyle adjustments, medication like sodium oxybate, and scheduled naps to improve daytime alertness and safety. Support includes multidisciplinary care involving neurologists, sleep specialists, mental health professionals, and patient education to enhance quality of life and reduce complications associated with falls or injuries during cataplexy episodes.
Narcolepsy and Cataplexy Infographic
 libterm.com
libterm.com