Thrombophlebitis refers to inflammation of a vein caused by a blood clot, commonly occurring in the legs and resulting in pain, swelling, and redness. Early diagnosis and treatment are essential to prevent complications such as deep vein thrombosis or pulmonary embolism, which can pose serious health risks. Discover the causes, symptoms, and effective management strategies in the rest of this article to protect your vascular health.
Table of Comparison
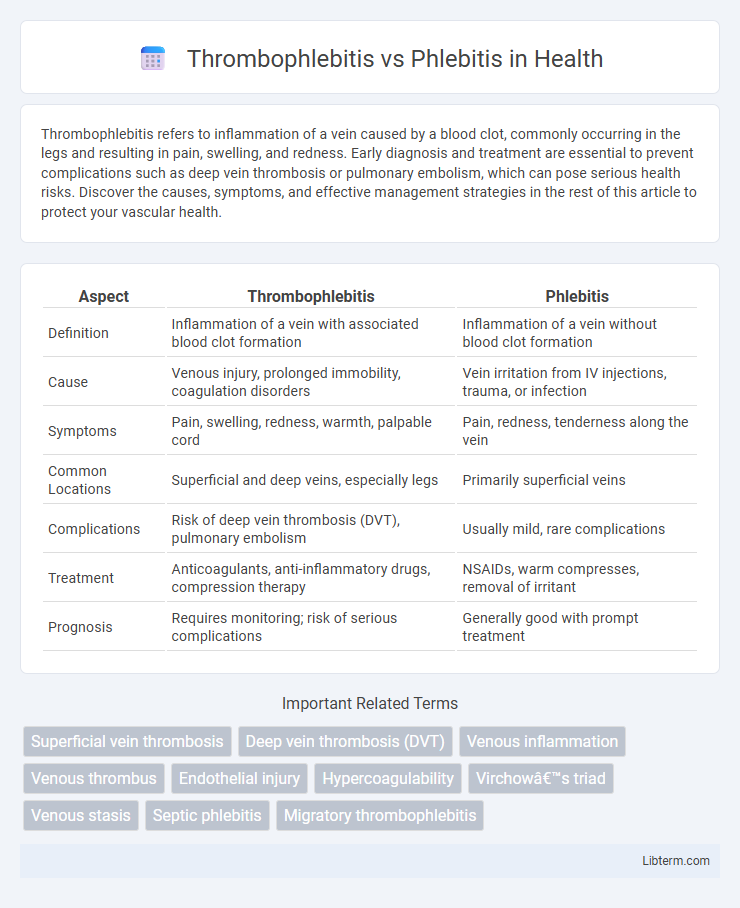
| Aspect | Thrombophlebitis | Phlebitis |
|---|---|---|
| Definition | Inflammation of a vein with associated blood clot formation | Inflammation of a vein without blood clot formation |
| Cause | Venous injury, prolonged immobility, coagulation disorders | Vein irritation from IV injections, trauma, or infection |
| Symptoms | Pain, swelling, redness, warmth, palpable cord | Pain, redness, tenderness along the vein |
| Common Locations | Superficial and deep veins, especially legs | Primarily superficial veins |
| Complications | Risk of deep vein thrombosis (DVT), pulmonary embolism | Usually mild, rare complications |
| Treatment | Anticoagulants, anti-inflammatory drugs, compression therapy | NSAIDs, warm compresses, removal of irritant |
| Prognosis | Requires monitoring; risk of serious complications | Generally good with prompt treatment |
Introduction to Thrombophlebitis and Phlebitis
Thrombophlebitis is the inflammation of a vein caused by a blood clot, often occurring in the legs and leading to pain, swelling, and redness. Phlebitis refers broadly to the inflammation of a vein without necessarily involving a clot, typically resulting from injury, infection, or irritation. Both conditions affect venous health, but thrombophlebitis carries a higher risk of complications due to clot formation.
Definition of Thrombophlebitis
Thrombophlebitis is the inflammation of a vein caused by a blood clot, typically occurring in the legs, and it can lead to complications such as deep vein thrombosis or pulmonary embolism. Phlebitis refers to vein inflammation without the presence of a clot, usually presenting with pain, redness, and swelling along the affected vein. Understanding the presence of a thrombus is critical to distinguishing thrombophlebitis from simple phlebitis for appropriate medical treatment and prevention of severe vascular complications.
Definition of Phlebitis
Phlebitis refers to the inflammation of a vein, typically occurring in superficial veins and characterized by redness, swelling, and tenderness along the affected vein. It is often caused by trauma, infection, or prolonged immobility, leading to irritation and swelling of the vein wall. Unlike thrombophlebitis, which involves both inflammation and clot formation, phlebitis primarily involves inflammation without significant thrombus development.
Key Differences Between Thrombophlebitis and Phlebitis
Thrombophlebitis involves inflammation of a vein accompanied by a blood clot, whereas phlebitis is inflammation without clot formation. Thrombophlebitis commonly presents with swelling, pain, and redness over a superficial vein, often in the legs, while phlebitis may cause similar symptoms but lacks the thrombotic component. Diagnosis of thrombophlebitis often requires ultrasound imaging to detect clots, distinguishing it from phlebitis, which is primarily diagnosed through clinical examination.
Causes and Risk Factors
Thrombophlebitis involves inflammation of a vein accompanied by a blood clot, often caused by prolonged immobility, varicose veins, or injury to the vein wall. Phlebitis refers to vein inflammation without clot formation, commonly triggered by infections, intravenous catheter use, or chemical irritation. Both conditions share risk factors such as venous stasis, trauma, and hypercoagulable states but differ in the presence of thrombosis in thrombophlebitis.
Common Symptoms and Clinical Presentation
Thrombophlebitis and phlebitis both present with localized inflammation, pain, redness, and swelling along the affected vein, typically in the legs. Thrombophlebitis is characterized by the presence of a blood clot causing vein hardening and increased tenderness, whereas phlebitis involves inflammation without clot formation. Common clinical symptoms include warmth, palpable cord-like veins, and tenderness, with thrombophlebitis often accompanied by signs of venous obstruction.
Diagnosis and Diagnostic Tools
Thrombophlebitis diagnosis primarily relies on Doppler ultrasound to detect blood clots and assess vein inflammation, while phlebitis diagnosis focuses on clinical examination and ultrasound for identifying vein wall inflammation without thrombosis. Blood tests such as D-dimer may support thrombophlebitis diagnosis by indicating coagulation activity, whereas phlebitis diagnosis depends more on patient history and physical signs like redness and tenderness. Imaging tools like venography or MRI are less common but can be used in complex cases to distinguish between thrombophlebitis and phlebitis.
Treatment Options and Management Strategies
Thrombophlebitis treatment primarily involves anticoagulants like heparin or warfarin to prevent clot extension and compression therapy to reduce inflammation and swelling. Phlebitis management typically includes nonsteroidal anti-inflammatory drugs (NSAIDs), warm compresses, and elevation to alleviate pain and inflammation. Both conditions benefit from lifestyle modifications such as mobility enhancement and avoiding prolonged immobility to reduce recurrence risk.
Potential Complications and Prognosis
Thrombophlebitis involves the formation of a blood clot in an inflamed vein, increasing the risk of deep vein thrombosis (DVT) and pulmonary embolism, which can lead to life-threatening complications. Phlebitis, primarily characterized by vein inflammation without clot formation, generally has a milder prognosis but can progress to thrombophlebitis if untreated. Early diagnosis and treatment are critical to reducing complications, with thrombophlebitis requiring more intensive management due to the higher potential for systemic effects and recurrence.
Prevention and Patient Education
Preventing thrombophlebitis and phlebitis involves maintaining adequate hydration, regular physical activity, and avoiding prolonged immobility to promote healthy blood circulation. Patient education emphasizes recognizing early symptoms such as localized redness, swelling, and warmth, encouraging prompt medical consultation for timely diagnosis and treatment. Teaching patients about proper catheter care and avoiding trauma to veins reduces the risk of inflammation and clot formation.
Thrombophlebitis Infographic
 libterm.com
libterm.com