Meningoencephalitis is a serious neurological condition characterized by inflammation of both the meninges and the brain, often caused by viral or bacterial infections. Early diagnosis and treatment are crucial to prevent long-term complications and improve recovery outcomes. Explore this article to understand the symptoms, causes, and effective management strategies for meningoencephalitis.
Table of Comparison
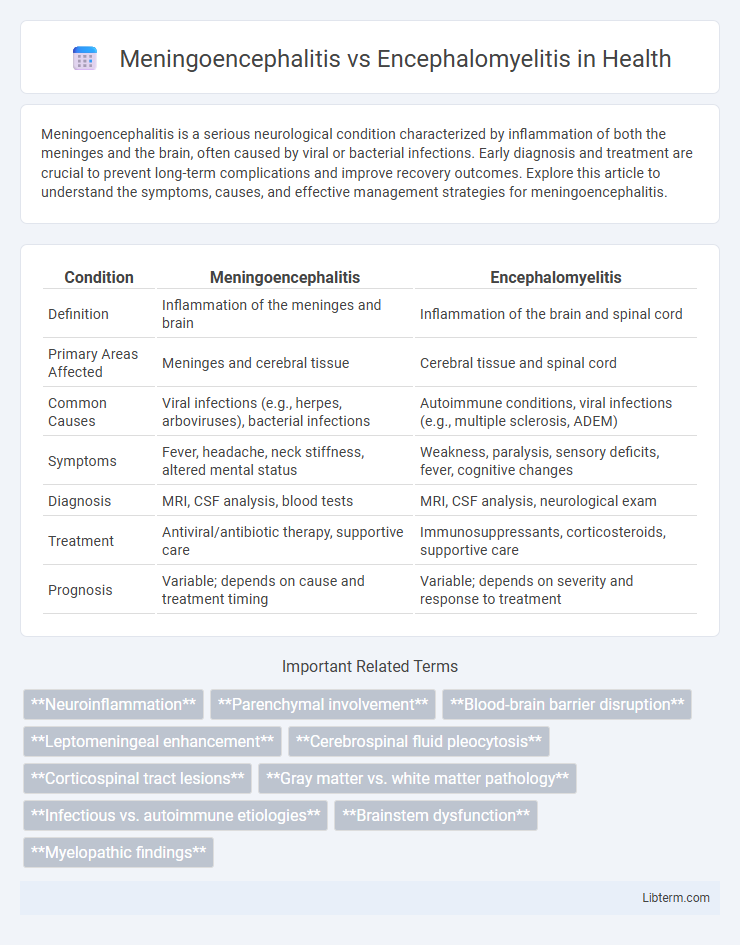
| Condition | Meningoencephalitis | Encephalomyelitis |
|---|---|---|
| Definition | Inflammation of the meninges and brain | Inflammation of the brain and spinal cord |
| Primary Areas Affected | Meninges and cerebral tissue | Cerebral tissue and spinal cord |
| Common Causes | Viral infections (e.g., herpes, arboviruses), bacterial infections | Autoimmune conditions, viral infections (e.g., multiple sclerosis, ADEM) |
| Symptoms | Fever, headache, neck stiffness, altered mental status | Weakness, paralysis, sensory deficits, fever, cognitive changes |
| Diagnosis | MRI, CSF analysis, blood tests | MRI, CSF analysis, neurological exam |
| Treatment | Antiviral/antibiotic therapy, supportive care | Immunosuppressants, corticosteroids, supportive care |
| Prognosis | Variable; depends on cause and treatment timing | Variable; depends on severity and response to treatment |
Introduction to Meningoencephalitis and Encephalomyelitis
Meningoencephalitis is an inflammatory condition affecting both the meninges and the brain parenchyma, often caused by viral or bacterial infections, leading to symptoms such as headache, fever, and altered mental status. Encephalomyelitis involves inflammation of the brain and spinal cord, frequently triggered by autoimmune responses or infections, resulting in neurological deficits like muscle weakness and sensory disturbances. Both conditions require prompt diagnosis and intervention to prevent severe neurological damage and improve patient outcomes.
Definitions and Key Differences
Meningoencephalitis is an inflammatory condition involving both the meninges and the brain parenchyma, often caused by viral or bacterial infections, while encephalomyelitis specifically refers to inflammation of the brain and spinal cord. Key differences include the anatomical regions affected: meningoencephalitis impacts the brain and its surrounding membranes, whereas encephalomyelitis extends inflammation to the spinal cord. Clinical presentations and diagnostic imaging techniques vary accordingly, with meningoencephalitis often showing meningeal irritation signs and encephalomyelitis exhibiting neurological deficits related to spinal cord involvement.
Epidemiology and Prevalence
Meningoencephalitis, an inflammation involving both the meninges and brain parenchyma, is often caused by viral infections such as herpes simplex virus and arboviruses, with incidence rates varying widely by region, especially in tropical and subtropical areas. Encephalomyelitis, characterized by inflammation of the brain and spinal cord, commonly results from autoimmune diseases or infections like acute disseminated encephalomyelitis (ADEM), showing higher prevalence in children and young adults predominantly in temperate climates. Epidemiological data indicate meningitis-related outbreaks are more frequent in developing countries, while encephalomyelitis cases are sporadic but significant due to their potential association with vaccination and post-infectious immune responses.
Causes and Risk Factors
Meningoencephalitis is primarily caused by viral infections such as herpes simplex virus and enteroviruses, with bacterial infections and autoimmune disorders also contributing to its occurrence. Encephalomyelitis often results from post-infectious autoimmune responses, including acute disseminated encephalomyelitis (ADEM), triggered by viral or bacterial infections and vaccinations. Risk factors for both conditions include immunosuppression, recent infections, and exposure to endemic regions where causative pathogens are prevalent.
Pathophysiology: How Each Condition Develops
Meningoencephalitis involves inflammation of both the meninges and brain tissue, primarily triggered by infectious agents such as viruses, bacteria, or fungi invading the central nervous system, leading to neuronal damage and immune response activation. Encephalomyelitis affects both the brain and spinal cord, frequently resulting from autoimmune reactions, infections, or post-infectious processes where immune-mediated inflammation causes demyelination and neural tissue injury. The pathophysiology of meningoencephalitis centers on infectious inflammation spreading from the meninges to the brain parenchyma, whereas encephalomyelitis involves immune-driven inflammatory mechanisms targeting neural structures across the brain and spinal cord.
Clinical Presentation and Symptoms
Meningoencephalitis presents with a combination of meningeal irritation signs such as neck stiffness, photophobia, and headache, alongside encephalitic symptoms including altered mental status, seizures, and focal neurological deficits. Encephalomyelitis primarily manifests with widespread inflammation involving both the brain and spinal cord, leading to symptoms like limb weakness, sensory disturbances, and autonomic dysfunction in addition to altered consciousness and cognitive impairment. Clinical differentiation relies on the predominance of meningeal versus spinal cord involvement, with meningoencephalitis showing more pronounced meningitis features and encephalomyelitis demonstrating extensive motor and sensory pathway deficits.
Diagnostic Approaches and Testing
Diagnostic approaches for meningoencephalitis and encephalomyelitis involve cerebrospinal fluid (CSF) analysis, magnetic resonance imaging (MRI), and serological testing. Meningoencephalitis typically shows elevated white blood cells and protein in CSF, while MRI reveals inflammation in both meninges and brain parenchyma. Encephalomyelitis diagnosis emphasizes MRI findings showing lesions in the brain and spinal cord, supported by CSF analysis detecting inflammatory markers and autoimmune antibodies.
Treatment Strategies and Management
Treatment strategies for meningoencephalitis primarily involve targeted antimicrobial or antiviral therapy based on the identified pathogen, along with corticosteroids to reduce inflammation and supportive care to address neurological symptoms. Management of encephalomyelitis focuses on immunosuppressive therapies such as high-dose corticosteroids, intravenous immunoglobulin (IVIG), or plasmapheresis to control autoimmune inflammation affecting both the brain and spinal cord. Both conditions require early diagnosis, close neurological monitoring, and multidisciplinary rehabilitation to minimize long-term neurological deficits.
Prognosis and Possible Complications
Meningoencephalitis often results in better prognosis if treated promptly, but complications such as seizures, cognitive impairment, and focal neurological deficits can persist, especially in cases involving infectious or autoimmune causes. Encephalomyelitis typically carries a more guarded prognosis due to the involvement of both the brain and spinal cord, with complications including paralysis, sensory disturbances, and chronic inflammation that may lead to long-term disability. Early diagnosis and targeted therapy significantly influence recovery outcomes and reduce the risk of severe neurological sequelae in both conditions.
Prevention and Future Research Directions
Meningoencephalitis prevention centers on vaccination, vector control, and prompt treatment of infections to reduce inflammation of the brain and meninges, while encephalomyelitis prevention emphasizes managing autoimmune triggers and infections that affect both the brain and spinal cord. Future research directions include exploring advanced immunomodulatory therapies, identifying novel biomarkers for early diagnosis, and developing targeted antiviral treatments to improve outcomes for both conditions. Innovations in neuroimaging and molecular diagnostics are essential to enhance understanding of pathophysiological mechanisms and tailor personalized interventions.
Meningoencephalitis Infographic
 libterm.com
libterm.com