Contamination poses significant risks to health, safety, and the environment by introducing harmful substances into air, water, or soil. Effective contamination control and prevention strategies are essential for maintaining clean ecosystems and protecting public well-being. Explore this article to learn how you can identify, manage, and reduce contamination effectively.
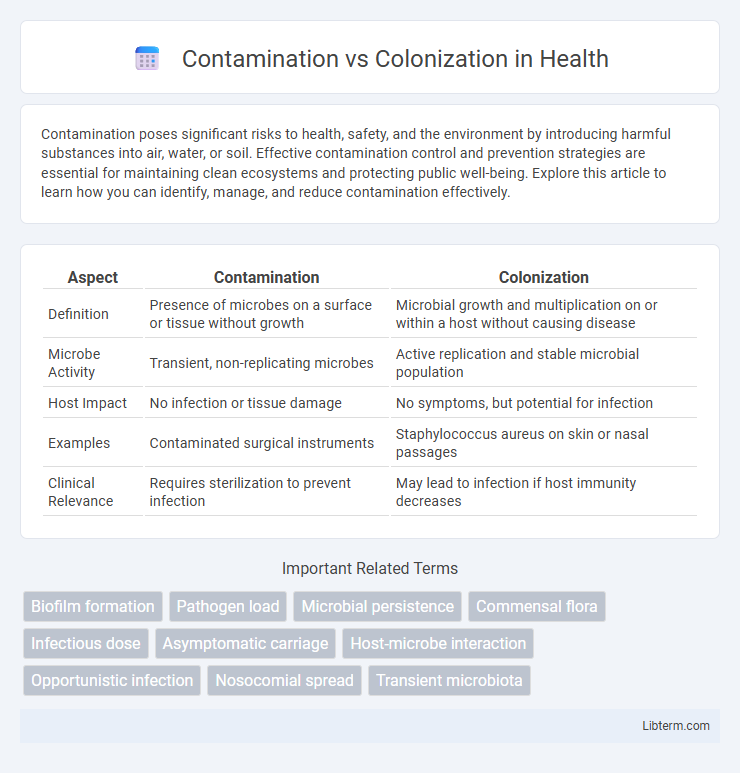
Table of Comparison
| Aspect | Contamination | Colonization |
|---|---|---|
| Definition | Presence of microbes on a surface or tissue without growth | Microbial growth and multiplication on or within a host without causing disease |
| Microbe Activity | Transient, non-replicating microbes | Active replication and stable microbial population |
| Host Impact | No infection or tissue damage | No symptoms, but potential for infection |
| Examples | Contaminated surgical instruments | Staphylococcus aureus on skin or nasal passages |
| Clinical Relevance | Requires sterilization to prevent infection | May lead to infection if host immunity decreases |
Understanding Contamination and Colonization
Contamination involves the presence of microorganisms on a surface or in a sample without multiplication or infection, often due to external exposure, whereas colonization refers to the growth and multiplication of microbes on or within a host without causing disease symptoms. Distinguishing contamination from colonization is crucial in clinical diagnostics to avoid false positives and ensure accurate treatment decisions. Understanding the microbial load and the context of sample collection helps differentiate transient contamination from stable colonization.
Key Differences Between Contamination and Colonization
Contamination refers to the presence of unwanted microorganisms on surfaces or materials without causing infection, whereas colonization involves microorganisms establishing and multiplying on or within a host without causing tissue damage. Contamination is often transient and can be eliminated through cleaning or sterilization, while colonization represents a more stable microbial presence that may lead to infection if the host's defenses are compromised. Understanding these distinctions is critical in clinical settings to prevent misdiagnosis and ensure appropriate treatment strategies.
Sources of Microbial Contamination
Sources of microbial contamination primarily include environmental surfaces, healthcare personnel, and medical devices, with pathogens often originating from air, water, and fomites. Colonization occurs when microbes establish themselves on body sites without causing disease, commonly from endogenous flora or transient microbes acquired through contact. Distinguishing contamination from colonization is crucial in clinical diagnostics to prevent misinterpretation of microbial presence, guiding appropriate infection control measures.
Mechanisms of Colonization in Hosts
Colonization in hosts involves the adherence of microorganisms to epithelial surfaces via specific adhesins binding to host cell receptors, enabling stable attachment. Biofilm formation further facilitates persistence by creating a protective matrix that resists host immune responses and antimicrobial agents. These mechanisms distinguish colonization from mere contamination, where microbes are transient and do not establish a stable presence.
Impact on Human Health
Contamination introduces harmful microorganisms or substances to a surface or environment, potentially causing immediate health risks through infection or toxicity. Colonization occurs when microorganisms establish themselves on or within the body without causing disease, often serving as reservoirs for opportunistic infections under weakened immunity. The distinction is critical in clinical settings to avoid misdiagnosis and ensure appropriate infection control measures, reducing the spread of healthcare-associated infections.
Diagnostic Criteria for Differentiation
Diagnostic criteria for differentiating contamination from colonization primarily involve microbial culture results, clinical presentation, and sample collection methods. Contamination is indicated by the presence of microorganisms in a sample without corresponding signs of infection or inflammation, often due to improper sampling techniques, whereas colonization is characterized by the persistent presence of microorganisms on or within body sites without causing disease. Quantitative cultures, host immune response markers, and consistent isolation of the same organism from multiple samples help distinguish colonization from contamination, guiding appropriate clinical management.
Clinical Significance of Each Process
Contamination involves the unintended presence of microorganisms on a surface or sample, often without causing infection, leading to false-positive clinical results and unnecessary treatments. Colonization refers to the presence of microorganisms on or within a host without tissue invasion or immune response, which can progress to infection depending on host immunity and microbial virulence. Differentiating contamination from colonization is crucial in clinical diagnostics to avoid misdiagnosis, guide appropriate antimicrobial therapy, and reduce antibiotic resistance.
Prevention Strategies for Contamination
Effective prevention of contamination centers on strict adherence to aseptic techniques, including thorough hand hygiene and sterilization of medical instruments. Environmental controls such as proper waste disposal, surface disinfection, and air filtration significantly reduce the risk of introducing contaminants in healthcare and laboratory settings. Regular training and compliance monitoring further ensure that contamination sources are minimized, maintaining sample and patient safety.
Managing Colonization in Healthcare Settings
Managing colonization in healthcare settings requires stringent infection control protocols, including routine screening and isolation of colonized patients to prevent the spread of multidrug-resistant organisms (MDROs). Hand hygiene compliance and environmental decontamination play critical roles in reducing bacterial reservoirs and minimizing transmission. Implementing antimicrobial stewardship programs helps limit unnecessary antibiotic use, which reduces selective pressure and the risk of converting colonization into active infection.
Importance in Infection Control and Public Health
Distinguishing contamination from colonization is crucial in infection control and public health to prevent misdiagnosis and inappropriate treatment. Contamination refers to the presence of microorganisms on surfaces or samples without causing infection, whereas colonization indicates microbial presence on or within a host without signs of disease but with potential for transmission. Accurate identification helps in implementing targeted hygiene practices, optimizing antimicrobial use, and reducing the spread of multidrug-resistant organisms in healthcare settings.
Contamination Infographic
 libterm.com
libterm.com