Peptic ulcer disease causes painful sores in the lining of your stomach or the first part of your small intestine, often due to infection with Helicobacter pylori or prolonged use of NSAIDs. Symptoms include burning stomach pain, bloating, and nausea, which can worsen if left untreated. Discover effective treatment options and lifestyle changes to manage peptic ulcer disease by reading the rest of the article.
Table of Comparison
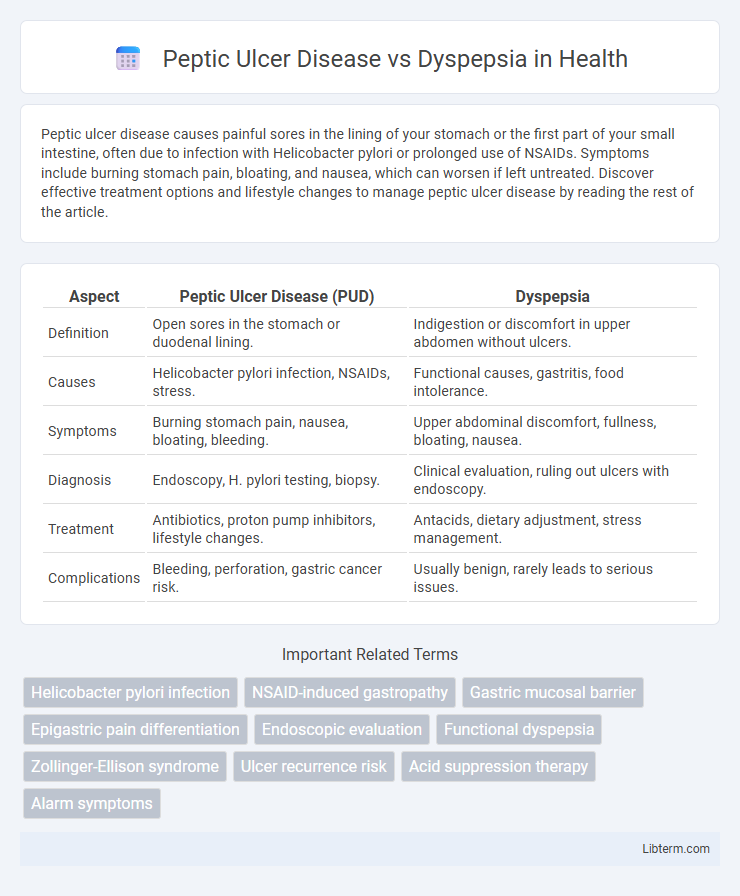
| Aspect | Peptic Ulcer Disease (PUD) | Dyspepsia |
|---|---|---|
| Definition | Open sores in the stomach or duodenal lining. | Indigestion or discomfort in upper abdomen without ulcers. |
| Causes | Helicobacter pylori infection, NSAIDs, stress. | Functional causes, gastritis, food intolerance. |
| Symptoms | Burning stomach pain, nausea, bloating, bleeding. | Upper abdominal discomfort, fullness, bloating, nausea. |
| Diagnosis | Endoscopy, H. pylori testing, biopsy. | Clinical evaluation, ruling out ulcers with endoscopy. |
| Treatment | Antibiotics, proton pump inhibitors, lifestyle changes. | Antacids, dietary adjustment, stress management. |
| Complications | Bleeding, perforation, gastric cancer risk. | Usually benign, rarely leads to serious issues. |
Introduction to Peptic Ulcer Disease and Dyspepsia
Peptic Ulcer Disease (PUD) is characterized by open sores that develop on the inner lining of the stomach or the upper part of the small intestine, primarily caused by Helicobacter pylori infection and prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs). Dyspepsia, commonly referred to as indigestion, encompasses a set of symptoms including upper abdominal discomfort, bloating, nausea, and early satiety, without an identifiable ulcer or structural cause. Differentiating PUD from functional dyspepsia is crucial for targeted treatment, as PUD involves mucosal damage whereas dyspepsia can be linked to motility disturbances or hypersensitivity in the gastrointestinal tract.
Defining Peptic Ulcer Disease
Peptic Ulcer Disease (PUD) is a condition characterized by the formation of open sores or ulcers in the lining of the stomach, duodenum, or esophagus caused primarily by Helicobacter pylori infection or prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs). Dyspepsia, often referred to as indigestion, involves recurring discomfort or pain in the upper abdomen without visible ulcers or eroded tissue upon diagnostic evaluation. While PUD presents with more specific symptoms such as epigastric pain relieved by food or antacids, dyspepsia symptoms are broader and less defined, making accurate diagnosis essential for targeted treatment.
Understanding Dyspepsia
Dyspepsia, commonly known as indigestion, encompasses a range of upper abdominal symptoms including bloating, nausea, and epigastric pain, often without a clear structural cause. Unlike Peptic Ulcer Disease (PUD), which involves mucosal erosion in the stomach or duodenum identified via endoscopy, dyspepsia can be functional, lacking visible ulcers but significantly impacting quality of life. Understanding dyspepsia requires distinguishing functional dyspepsia from organic diseases using clinical evaluation, Helicobacter pylori testing, and sometimes endoscopic examination to guide appropriate management.
Key Clinical Differences
Peptic Ulcer Disease (PUD) is characterized by a well-defined mucosal ulcer in the stomach or duodenum confirmed by endoscopy, often causing localized epigastric pain worsened by fasting and relieved by eating or antacids, whereas Dyspepsia presents with nonspecific upper abdominal discomfort or fullness without visible mucosal damage. PUD frequently involves complications such as bleeding or perforation, indicated by signs like melena or hematemesis, while Dyspepsia typically lacks systemic features and severe complications. Helicobacter pylori infection and NSAID use are common etiological factors in PUD, which respond to targeted eradication therapy, contrasting with Dyspepsia's functional origin requiring symptom management.
Causes and Risk Factors
Peptic Ulcer Disease (PUD) is primarily caused by Helicobacter pylori infection and chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs), with smoking and excessive alcohol intake as significant risk factors. Dyspepsia, often resulting from functional gastrointestinal disorders, may be triggered by factors such as stress, dietary habits, and certain medications but lacks a definitive structural cause like ulcers. Both conditions share overlapping symptoms, yet distinguishing their causes is crucial for targeted treatment and management.
Diagnostic Approaches
Peptic Ulcer Disease (PUD) diagnosis involves endoscopic evaluation to identify mucosal erosions or ulcers in the stomach or duodenum, which provides definitive evidence and allows biopsy to exclude malignancy or Helicobacter pylori infection. Dyspepsia diagnosis often starts with non-invasive tests such as H. pylori breath or stool antigen tests and may include upper gastrointestinal endoscopy if alarm symptoms like weight loss, anemia, or gastrointestinal bleeding are present. Imaging studies and laboratory tests support differential diagnosis, distinguishing functional dyspepsia from organic causes including PUD and gastroesophageal reflux disease.
Symptom Comparison
Peptic Ulcer Disease (PUD) typically presents with localized epigastric pain described as burning or gnawing, often relieved by food or antacids, whereas dyspepsia encompasses a broader range of upper abdominal symptoms such as fullness, bloating, and nausea without consistent ulcerative lesions. In PUD, pain episodes can be nocturnal and recur cyclically, while dyspepsia symptoms are generally more chronic and less specific. Both conditions may share symptoms like upper abdominal discomfort, but endoscopic findings differentiate PUD's mucosal damage from the functional or non-ulcer-related origin of dyspepsia.
Treatment Strategies
Peptic Ulcer Disease (PUD) treatment primarily involves proton pump inhibitors (PPIs) to reduce gastric acid secretion and antibiotics to eradicate Helicobacter pylori infection, which is a major causative factor. Dyspepsia management focuses on lifestyle modifications, antacids, H2-receptor antagonists, and prokinetic agents to alleviate symptoms without necessarily targeting ulcer healing. In refractory cases of functional dyspepsia, low-dose tricyclic antidepressants or psychological therapies may be considered to restore gastrointestinal function and improve patient quality of life.
Complications and Prognosis
Peptic Ulcer Disease (PUD) can lead to serious complications such as bleeding, perforation, and gastric obstruction, significantly impacting morbidity and requiring urgent medical intervention. Dyspepsia, often functional or related to mild gastritis, generally has a benign prognosis with minimal risk of severe complications. Early diagnosis and appropriate treatment of PUD improve prognosis, whereas dyspepsia management focuses on symptom control and lifestyle modifications.
Prevention and Lifestyle Modifications
Peptic ulcer disease prevention centers on avoiding Helicobacter pylori infection through proper hygiene and minimizing NSAID use, while lifestyle modifications include quitting smoking, limiting alcohol consumption, and managing stress to promote mucosal healing. Dyspepsia prevention emphasizes dietary adjustments such as avoiding spicy, fatty, and acidic foods that trigger symptoms, coupled with regular meal patterns and weight management to reduce gastric discomfort. Both conditions benefit from reducing caffeine intake and adopting a balanced diet rich in fiber and antioxidants to support gastrointestinal health.
Peptic Ulcer Disease Infographic
 libterm.com
libterm.com