Fibrillation refers to rapid, irregular contractions of muscle fibers, most commonly seen in the heart's atria or ventricles, disrupting normal rhythm and impairing efficient blood flow. Understanding its causes, symptoms, and treatment options is crucial for preventing complications such as stroke or heart failure. Explore the rest of this article to learn how fibrillation may affect Your health and the best ways to manage it.
Table of Comparison
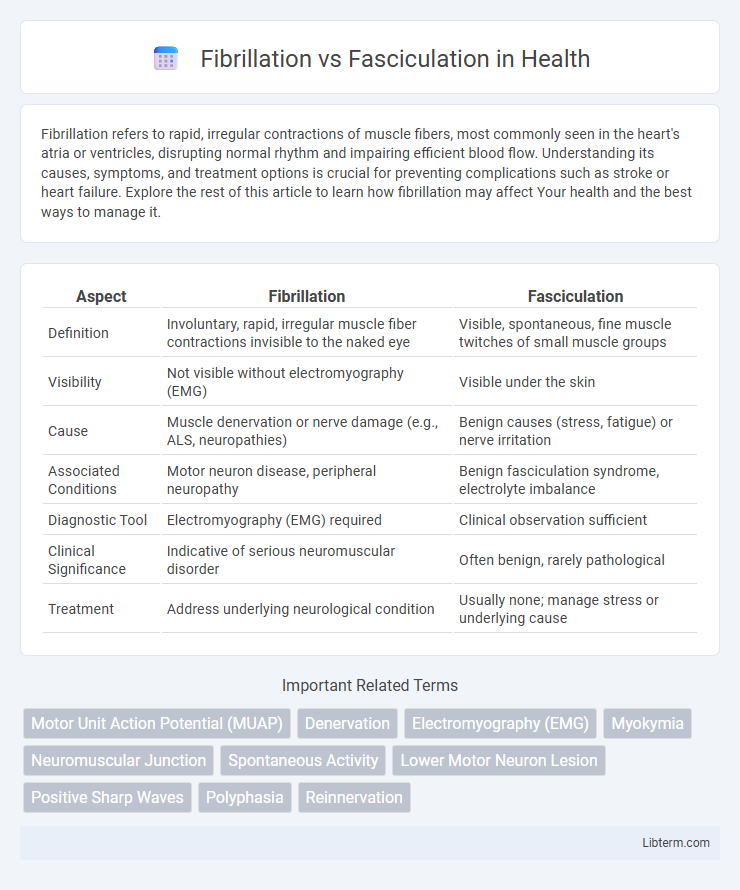
| Aspect | Fibrillation | Fasciculation |
|---|---|---|
| Definition | Involuntary, rapid, irregular muscle fiber contractions invisible to the naked eye | Visible, spontaneous, fine muscle twitches of small muscle groups |
| Visibility | Not visible without electromyography (EMG) | Visible under the skin |
| Cause | Muscle denervation or nerve damage (e.g., ALS, neuropathies) | Benign causes (stress, fatigue) or nerve irritation |
| Associated Conditions | Motor neuron disease, peripheral neuropathy | Benign fasciculation syndrome, electrolyte imbalance |
| Diagnostic Tool | Electromyography (EMG) required | Clinical observation sufficient |
| Clinical Significance | Indicative of serious neuromuscular disorder | Often benign, rarely pathological |
| Treatment | Address underlying neurological condition | Usually none; manage stress or underlying cause |
Introduction to Fibrillation and Fasciculation
Fibrillation and fasciculation are both involuntary muscle activities often associated with neurological conditions. Fibrillation refers to rapid, irregular muscle fiber contractions detectable only via electromyography, indicating muscle denervation or disease. Fasciculation consists of visible, spontaneous muscle twitches caused by spontaneous discharge of a motor unit, commonly linked to benign or pathological processes such as motor neuron diseases.
Key Definitions: Fibrillation vs Fasciculation
Fibrillation refers to rapid, irregular, and unsynchronized muscle fiber contractions often detected only via electromyography, indicating muscle or nerve pathology. Fasciculation consists of spontaneous, visible muscle twitches caused by involuntary activation of individual motor units, commonly associated with benign conditions or motor neuron diseases. Differentiating fibrillation from fasciculation is crucial for diagnosing neuromuscular disorders.
Causes of Fibrillation
Fibrillation is caused by nerve damage or disorders affecting the motor neurons, such as amyotrophic lateral sclerosis (ALS), peripheral neuropathy, or muscle denervation following injury. This abnormal spontaneous muscle fiber activity occurs due to disrupted nerve signals leading to uncoordinated contractions. Unlike fasciculations, which stem from superficial nerve irritation, fibrillations indicate more profound neuromuscular pathology.
Causes of Fasciculation
Fasciculation causes primarily include nerve irritation, muscle fatigue, electrolyte imbalances, and certain medications, which lead to involuntary muscle twitches noticeable under the skin. Unlike fibrillation, which originates from spontaneous activity of individual muscle fibers often linked to nerve injury or neuromuscular diseases, fasciculations are typically benign and stem from peripheral nerve hyperexcitability. Common triggers such as stress, caffeine intake, and focal nerve compression contribute to the development of fasciculations without significant muscle weakness.
Clinical Presentation: Symptoms Compared
Fibrillation presents clinically with involuntary, fine, and rapid muscle fiber contractions that are typically not visible but can be detected by electromyography. Fasciculations manifest as visible, spontaneous, brief muscle twitches affecting small groups of muscle fibers, often causing a rippling effect under the skin. Patients with fibrillation often experience muscle weakness and atrophy, while those with fasciculations may have minimal to no muscle weakness but report twitching sensations.
Diagnostic Criteria and Tools
Fibrillation refers to spontaneous, irregular muscle fiber contractions detected primarily through electromyography (EMG), indicating denervation at the muscle fiber level often seen in conditions like amyotrophic lateral sclerosis (ALS) or peripheral neuropathy. Fasciculation involves involuntary muscle twitching of entire motor units, observed clinically and confirmed by EMG, typically associated with benign fasciculation syndrome or motor neuron disease. Diagnostic criteria rely heavily on EMG patterns: fibrillations appear as brief, spontaneous, irregular potentials, while fasciculations present as larger, rhythmic discharges corresponding to motor unit activity.
Underlying Neurological Mechanisms
Fibrillation refers to spontaneous, irregular muscle fiber contractions caused by denervation or motor neuron disease, indicating disruption at the neuromuscular junction or anterior horn cells. Fasciculation, characterized by visible, involuntary muscle twitches, results from hyperexcitability of the motor neuron or axonal irritation without complete loss of nerve supply. Both phenomena reflect distinct pathological processes in peripheral nerves, with fibrillations signaling active muscle fiber denervation and fasciculations indicating motor neuron membrane instability.
Significance in Neuromuscular Disorders
Fibrillation and fasciculation both indicate abnormal muscle activity but differ significantly in their clinical implications for neuromuscular disorders. Fibrillation potentials, detected via electromyography, typically suggest active muscle fiber denervation seen in diseases like amyotrophic lateral sclerosis (ALS) and peripheral neuropathies. Fasciculations, often visible as muscle twitches, can occur in benign conditions but when persistent and widespread may signal motor neuron disease or spinal muscular atrophy, highlighting their diagnostic significance.
Treatment Approaches and Management
Treatment approaches for fibrillation primarily involve addressing the underlying neurological disorders, often using anticholinesterase agents and immunosuppressants in cases like myasthenia gravis. Fasciculations typically require management of the root cause, such as electrolyte imbalances or nerve irritation, and may include muscle relaxants or magnesium supplements. Both conditions benefit from symptomatic relief through physical therapy and regular monitoring to prevent progression or complications.
Prognosis and Long-term Implications
Fibrillation refers to spontaneous, irregular muscle fiber contractions seen primarily in denervated muscle and is often indicative of ongoing nerve damage, with prognosis dependent on the underlying cause such as peripheral neuropathy or motor neuron disease. Fasciculations are visible, involuntary muscle twitches stemming from spontaneous discharge of a motor neuron or its axon, generally benign when isolated but possibly signaling early neurodegenerative conditions like amyotrophic lateral sclerosis (ALS) when persistent. Long-term implications of fibrillation often include muscle atrophy and weakness without timely intervention, whereas persistent fasciculations warrant neurological evaluation to monitor potential progression, although many cases remain stable without significant functional decline.
Fibrillation Infographic
 libterm.com
libterm.com