Thrombocythemia causes an excessively high platelet count, increasing the risk of clot formation, while thrombocytopenia results in dangerously low platelet levels, leading to excessive bleeding and bruising. Both conditions require careful diagnosis and management to prevent serious complications. Discover more about their symptoms, causes, and treatments in the rest of the article.
Table of Comparison
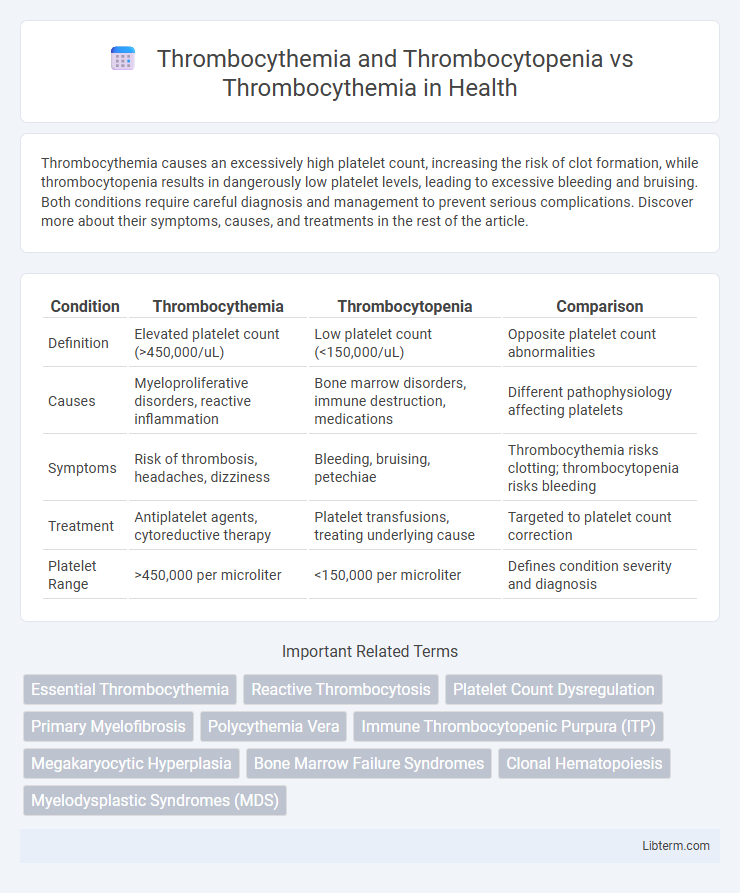
| Condition | Thrombocythemia | Thrombocytopenia | Comparison |
|---|---|---|---|
| Definition | Elevated platelet count (>450,000/uL) | Low platelet count (<150,000/uL) | Opposite platelet count abnormalities |
| Causes | Myeloproliferative disorders, reactive inflammation | Bone marrow disorders, immune destruction, medications | Different pathophysiology affecting platelets |
| Symptoms | Risk of thrombosis, headaches, dizziness | Bleeding, bruising, petechiae | Thrombocythemia risks clotting; thrombocytopenia risks bleeding |
| Treatment | Antiplatelet agents, cytoreductive therapy | Platelet transfusions, treating underlying cause | Targeted to platelet count correction |
| Platelet Range | >450,000 per microliter | <150,000 per microliter | Defines condition severity and diagnosis |
Introduction to Thrombocythemia and Thrombocytopenia
Thrombocythemia and thrombocytopenia represent opposite abnormalities in platelet counts, with thrombocythemia characterized by an excessive number of platelets leading to increased clotting risk, while thrombocytopenia involves a dangerously low platelet count resulting in bleeding tendencies. Essential thrombocythemia, a myeloproliferative disorder, causes sustained platelet overproduction, often linked to mutations such as JAK2 V617F, MPL, or CALR. In contrast, thrombocytopenia may result from bone marrow disorders, autoimmune diseases, or medication-induced platelet destruction, necessitating distinct diagnostic and therapeutic approaches.
Understanding Platelet Disorders
Thrombocythemia and thrombocytopenia represent opposing platelet disorders characterized by abnormal platelet counts, where thrombocythemia involves an excessive number of platelets causing increased clotting risk, while thrombocytopenia indicates a deficiency of platelets leading to bleeding complications. Understanding these disorders requires evaluating bone marrow function and platelet production, often through complete blood count (CBC) tests and bone marrow biopsies to distinguish between reactive and essential thrombocythemia. Accurate diagnosis shapes treatment strategies, emphasizing platelet count regulation via medications like hydroxyurea for thrombocythemia or platelet transfusions and corticosteroids for thrombocytopenia.
What is Thrombocythemia?
Thrombocythemia is a blood disorder characterized by an abnormally high platelet count, often exceeding 450,000 platelets per microliter of blood, which increases the risk of clotting complications such as stroke or deep vein thrombosis. Unlike thrombocytopenia, where platelet levels are dangerously low, thrombocythemia causes excessive platelet production typically due to bone marrow abnormalities, including essential thrombocythemia or secondary reactive thrombocytosis. Accurate diagnosis requires blood tests and bone marrow examination to differentiate primary thrombocythemia from thrombocytopenia conditions and manage potential thrombotic or bleeding risks effectively.
Primary vs Secondary Thrombocythemia
Primary thrombocythemia, also known as essential thrombocythemia, is a myeloproliferative disorder characterized by clonal proliferation of megakaryocytes leading to persistent high platelet counts without an identifiable cause. Secondary thrombocythemia occurs due to reactive processes such as inflammation, infection, or iron deficiency, resulting in elevated platelet levels as a physiological response. Thrombocytopenia, in contrast, involves abnormally low platelet counts caused by diverse factors including bone marrow suppression, autoimmune destruction, or increased platelet consumption.
Defining Thrombocytopenia: Key Differences
Thrombocythemia is characterized by an abnormally high platelet count, whereas thrombocytopenia involves a significantly low platelet count, leading to increased bleeding risks. Key differences include thrombocytopenia's association with conditions like bone marrow failure, autoimmune diseases, or medication effects, while thrombocythemia often results from myeloproliferative disorders such as essential thrombocythemia or reactive responses. Accurate diagnosis involves platelet count measurement, bone marrow examination, and genetic testing to distinguish between these platelet disorders.
Causes and Risk Factors: Thrombocythemia vs Thrombocytopenia
Thrombocythemia is primarily caused by myeloproliferative disorders such as essential thrombocythemia, leading to excessive platelet production, while secondary causes include inflammation, infection, or iron deficiency. Thrombocytopenia results from factors like bone marrow suppression, autoimmune diseases (e.g., immune thrombocytopenic purpura), viral infections, or medication-induced platelet destruction. Risk factors for thrombocythemia include genetic mutations like JAK2, MPL, or CALR, whereas thrombocytopenia risk factors encompass chemotherapy, HIV infection, liver disease, and hypersplenism.
Clinical Manifestations: Symptoms Comparison
Thrombocythemia presents with symptoms such as headaches, dizziness, and an increased risk of thrombosis due to elevated platelet counts, while thrombocytopenia typically manifests with petechiae, easy bruising, and prolonged bleeding from minor trauma because of reduced platelet levels. The contrasting platelet abnormalities result in distinct clinical manifestations; thrombocythemia leads to clotting complications, whereas thrombocytopenia causes hemorrhagic issues. Monitoring platelet counts and associated symptoms is crucial for differential diagnosis and targeted treatment in patients with these platelet disorders.
Diagnostic Approaches for Platelet Abnormalities
Diagnostic approaches for platelet abnormalities such as thrombocythemia and thrombocytopenia rely on comprehensive blood tests including complete blood counts (CBC) and peripheral blood smears to quantify platelet levels and assess morphology. Advanced diagnostics involve bone marrow biopsies and genetic testing, particularly for mutations in the JAK2, CALR, or MPL genes, which are frequently associated with essential thrombocythemia. Platelet function tests and coagulation profiles further aid in differentiating between reactive causes and primary myeloproliferative disorders, ensuring accurate classification and treatment strategies.
Treatment Options and Management Strategies
Thrombocythemia requires treatment strategies focused on reducing elevated platelet counts through medications such as hydroxyurea, anagrelide, or low-dose aspirin to prevent clot formation and related complications. In contrast, thrombocytopenia management prioritizes addressing underlying causes and raising platelet levels via corticosteroids, immunoglobulin therapy, or platelet transfusions to reduce bleeding risk. Tailored approaches for essential thrombocythemia versus secondary thrombocytopenia emphasize balancing thrombotic versus hemorrhagic risks based on platelet count abnormalities and patient-specific factors.
Prognosis and Long-Term Outcomes
Thrombocythemia, characterized by elevated platelet counts, generally presents a variable prognosis depending on whether it is essential or secondary, with essential thrombocythemia carrying a risk of thrombotic events but often manageable with treatment. Thrombocytopenia, defined by low platelet counts, usually involves higher risks of bleeding complications and can lead to more severe long-term outcomes, especially if caused by underlying disorders such as bone marrow failure or autoimmune diseases. Compared to thrombocythemia, thrombocytopenia typically requires more intensive monitoring and intervention to prevent significant morbidity and mortality.
Thrombocythemia and Thrombocytopenia Infographic
 libterm.com
libterm.com