Exudate is a fluid rich in proteins and cellular debris that oozes from blood vessels due to inflammation or injury. It plays a crucial role in the body's healing process by transporting immune cells to the affected area. Discover how understanding exudate can enhance your wound care knowledge by reading the rest of the article.
Table of Comparison
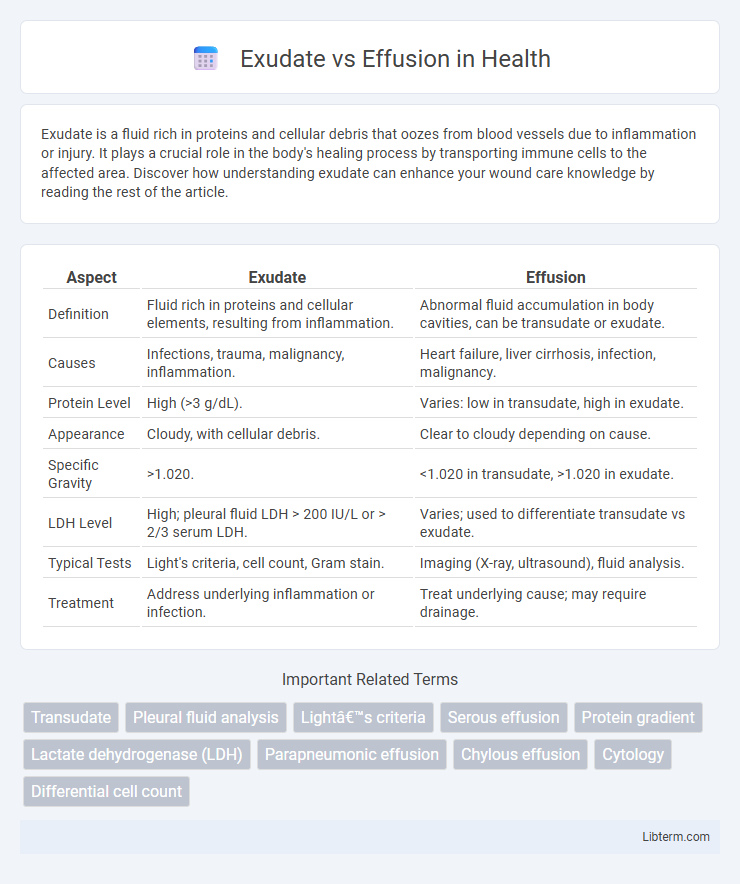
| Aspect | Exudate | Effusion |
|---|---|---|
| Definition | Fluid rich in proteins and cellular elements, resulting from inflammation. | Abnormal fluid accumulation in body cavities, can be transudate or exudate. |
| Causes | Infections, trauma, malignancy, inflammation. | Heart failure, liver cirrhosis, infection, malignancy. |
| Protein Level | High (>3 g/dL). | Varies: low in transudate, high in exudate. |
| Appearance | Cloudy, with cellular debris. | Clear to cloudy depending on cause. |
| Specific Gravity | >1.020. | <1.020 in transudate, >1.020 in exudate. |
| LDH Level | High; pleural fluid LDH > 200 IU/L or > 2/3 serum LDH. | Varies; used to differentiate transudate vs exudate. |
| Typical Tests | Light's criteria, cell count, Gram stain. | Imaging (X-ray, ultrasound), fluid analysis. |
| Treatment | Address underlying inflammation or infection. | Treat underlying cause; may require drainage. |
Introduction to Exudate and Effusion
Exudate is a protein-rich fluid typically resulting from inflammation and characterized by high cellular content and elevated specific gravity above 1.020. Effusion refers to the abnormal accumulation of fluid in body cavities, which can be either transudate or exudate, depending on its composition and underlying pathology. Distinguishing between exudate and transudate effusions is essential for diagnosing conditions such as infections, malignancies, or systemic diseases.
Defining Exudate: Key Characteristics
Exudate is a type of fluid accumulation characterized by high protein content, elevated lactate dehydrogenase (LDH) levels, and specific gravity greater than 1.020, distinguishing it from transudate and simple effusion. It typically results from inflammation, infection, or malignancy causing increased capillary permeability. The presence of cellular elements such as leukocytes and often a cloudy appearance further define exudate in clinical diagnosis.
Understanding Effusion: Types and Causes
Effusion is the abnormal accumulation of fluid in body cavities, commonly classified as transudate or exudate based on protein content and cellularity, which helps distinguish underlying causes. Transudative effusions usually result from systemic conditions like heart failure or cirrhosis, causing fluid imbalance without inflammation, while exudative effusions arise from local factors such as infections, malignancies, or inflammatory diseases that increase vascular permeability. Identifying the type and cause of effusion through diagnostic tests like pleural fluid analysis, including Light's criteria, is crucial for targeted treatment and management.
Pathophysiology: How Exudate and Effusion Develop
Exudates develop due to increased vascular permeability caused by inflammation, leading to protein-rich fluid leakage from blood vessels into surrounding tissues or cavities. Effusions form as a result of imbalances in hydrostatic and oncotic pressures, often related to systemic conditions such as heart failure, liver cirrhosis, or nephrotic syndrome, resulting in protein-poor fluid accumulation. The pathophysiology of exudate involves active endothelial injury and inflammatory cell recruitment, whereas effusion typically stems from passive transudation without direct inflammatory damage.
Common Clinical Presentations
Exudates commonly present in conditions such as infections, malignancies, and inflammatory diseases characterized by localized inflammation or tissue injury, often causing pleural effusion with high protein content and cellular debris. Effusions are typically associated with systemic factors like congestive heart failure, cirrhosis, or nephrotic syndrome, leading to transudative fluid accumulation with low protein concentration and minimal cellularity. Clinically, exudative effusions usually cause symptoms like fever, chest pain, and dyspnea, whereas transudative effusions present more insidiously with progressive dyspnea and signs of underlying systemic illness.
Diagnostic Criteria: Differentiating Exudate from Effusion
Exudate and effusion are differentiated based on their diagnostic criteria, particularly fluid analysis including protein concentration, lactate dehydrogenase (LDH) levels, and cell counts. Exudates typically present with a pleural fluid protein to serum protein ratio greater than 0.5, pleural fluid LDH greater than two-thirds of the upper limit of normal serum LDH, and higher nucleated cell counts indicating inflammation or malignancy. Effusions, often transudates, show lower protein ratios and LDH values, reflecting systemic conditions like heart failure or cirrhosis, rather than local pleural pathology.
Laboratory Tests and Imaging Techniques
Laboratory tests for exudate typically reveal high protein content, elevated lactate dehydrogenase (LDH) levels, and increased white blood cell count, indicating inflammation or infection, whereas effusion fluid often shows lower protein and LDH levels consistent with transudative processes. Imaging techniques such as chest X-ray and ultrasound help detect the presence and distribution of pleural fluid, with ultrasound providing superior sensitivity in differentiating between exudate and effusion by assessing septations and fluid characteristics. Computed tomography (CT) scans offer detailed visualization of associated pleural or pulmonary pathology, aiding in distinguishing exudative causes like malignancy or infection from transudative effusions related to systemic conditions.
Underlying Medical Conditions
Exudate typically indicates underlying inflammatory or infectious conditions such as pneumonia, tuberculosis, or malignancies that increase capillary permeability. Effusion often results from systemic diseases like congestive heart failure, cirrhosis, or nephrotic syndrome, leading to fluid accumulation due to imbalanced hydrostatic or oncotic pressures. Differentiating exudate from effusion helps identify the root cause and guides appropriate medical management.
Treatment Approaches and Management
Treatment approaches for exudate primarily focus on addressing the underlying cause, such as infections, malignancies, or inflammatory conditions, often involving antibiotics, anti-inflammatory agents, or oncologic therapies. Effusion management typically involves therapeutic drainage through thoracentesis or paracentesis to relieve symptoms, alongside addressing systemic issues like heart failure or liver cirrhosis with diuretics and supportive care. Both conditions require careful monitoring of fluid re-accumulation, with repeat procedures or surgical interventions like pleurodesis considered in refractory cases.
Prognosis and Complications
Exudates often indicate underlying inflammation or malignancy, leading to a variable prognosis depending on the cause, with complications such as infection, fibrosis, or persistent fluid accumulation. Effusions, typically transudates, usually reflect systemic conditions like heart failure or liver cirrhosis, with prognosis tied to managing the primary disease and fewer complications unless untreated. Both require accurate diagnosis to guide treatment and prevent complications like respiratory compromise or recurrent effusions.
Exudate Infographic
 libterm.com
libterm.com