Endocarditis is a serious infection of the heart's inner lining, usually caused by bacteria or fungi entering the bloodstream and attaching to damaged heart valves. Symptoms often include fever, fatigue, and heart murmur, requiring prompt medical diagnosis to prevent severe complications such as heart failure. Discover more about the causes, symptoms, and effective treatments for endocarditis in the rest of the article.
Table of Comparison
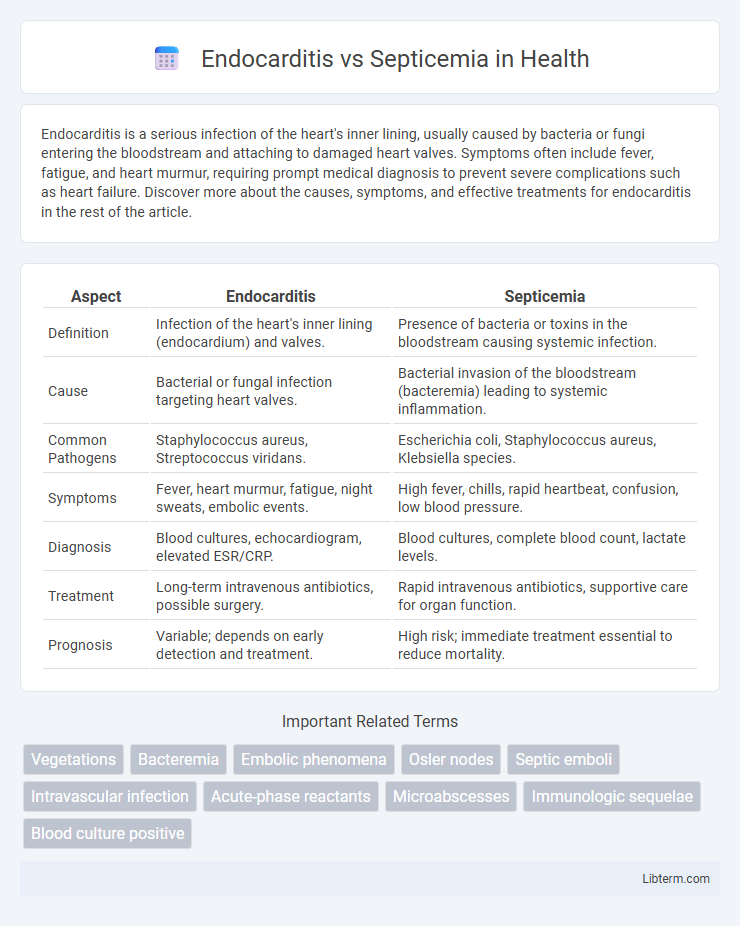
| Aspect | Endocarditis | Septicemia |
|---|---|---|
| Definition | Infection of the heart's inner lining (endocardium) and valves. | Presence of bacteria or toxins in the bloodstream causing systemic infection. |
| Cause | Bacterial or fungal infection targeting heart valves. | Bacterial invasion of the bloodstream (bacteremia) leading to systemic inflammation. |
| Common Pathogens | Staphylococcus aureus, Streptococcus viridans. | Escherichia coli, Staphylococcus aureus, Klebsiella species. |
| Symptoms | Fever, heart murmur, fatigue, night sweats, embolic events. | High fever, chills, rapid heartbeat, confusion, low blood pressure. |
| Diagnosis | Blood cultures, echocardiogram, elevated ESR/CRP. | Blood cultures, complete blood count, lactate levels. |
| Treatment | Long-term intravenous antibiotics, possible surgery. | Rapid intravenous antibiotics, supportive care for organ function. |
| Prognosis | Variable; depends on early detection and treatment. | High risk; immediate treatment essential to reduce mortality. |
Introduction to Endocarditis and Septicemia
Endocarditis is an infection of the inner lining of the heart chambers and valves caused by bacteria or fungi, leading to inflammation and potential heart damage. Septicemia, also known as blood poisoning, occurs when bacteria enter the bloodstream, triggering a systemic inflammatory response that can cause sepsis and organ failure. Both conditions require prompt medical diagnosis and treatment to prevent severe complications and improve patient outcomes.
Definition and Overview
Endocarditis is an infection of the inner lining of the heart chambers and valves, commonly caused by bacteria entering the bloodstream and attaching to damaged heart tissue. Septicemia, also known as blood poisoning, is a systemic infection where bacteria or their toxins circulate in the bloodstream, leading to widespread inflammation and potentially sepsis. Both conditions are severe infections, but endocarditis specifically affects heart structures, while septicemia involves a generalized invasion of the bloodstream.
Causes and Risk Factors
Endocarditis is primarily caused by bacterial infection of the heart valves or endocardium, often linked to risk factors such as pre-existing heart conditions, intravenous drug use, and invasive medical procedures. Septicemia, or blood poisoning, results from the presence of harmful bacteria or their toxins in the bloodstream, frequently triggered by infections like pneumonia, urinary tract infections, or surgical wounds. Both conditions share risk factors including weakened immune systems, chronic illnesses, and prolonged hospitalization, which increase susceptibility to severe bacterial infections.
Pathophysiology Differences
Endocarditis is characterized by the infection and inflammation of the heart's inner lining, particularly affecting the heart valves, leading to vegetation formation composed of bacteria, fibrin, and cellular debris. Septicemia involves the systemic spread of pathogens and their toxins through the bloodstream, triggering a widespread inflammatory response and potentially causing multiple organ dysfunction. The key pathophysiological difference lies in endocarditis being a localized infection with potential embolic complications, whereas septicemia represents a generalized bloodstream infection causing systemic inflammation and sepsis.
Common Signs and Symptoms
Endocarditis commonly presents with fever, heart murmurs, fatigue, and petechiae, along with symptoms such as night sweats and unexplained weight loss. Septicemia is characterized by systemic signs including high fever, chills, rapid breathing, and confusion, often accompanied by low blood pressure and organ dysfunction. Both conditions share fever and malaise but differ as endocarditis primarily affects the heart valves while septicemia causes widespread infection in the bloodstream.
Diagnostic Approaches
Endocarditis diagnosis primarily involves echocardiography, blood cultures, and the Modified Duke Criteria to detect vegetations and causative pathogens on heart valves. Septicemia diagnosis relies on blood cultures, complete blood counts, and biomarkers like procalcitonin to identify systemic bacterial infection and inflammation. Advanced molecular diagnostic techniques such as polymerase chain reaction (PCR) help differentiate the infectious agents in both conditions for targeted treatment.
Treatment Strategies
Treatment strategies for endocarditis primarily involve prolonged courses of intravenous antibiotics tailored to the causative bacteria, often requiring 4 to 6 weeks of therapy to eradicate infection from heart valves. In cases of septicemia, rapid administration of broad-spectrum intravenous antibiotics is critical, with adjustments made based on blood culture results to target specific pathogens and prevent systemic organ failure. Surgical intervention may be necessary in endocarditis to repair or replace damaged heart valves, whereas management of septicemia focuses on supportive care, including fluid resuscitation and organ support in intensive care units.
Complications Associated
Endocarditis can lead to severe complications such as heart valve damage, heart failure, and systemic embolism, increasing the risk of stroke and organ infarction. Septicemia frequently results in widespread inflammation causing septic shock, multi-organ failure, and disseminated intravascular coagulation (DIC). Both conditions demand prompt medical intervention to prevent life-threatening outcomes and irreversible tissue damage.
Prognosis and Outcomes
Endocarditis prognosis varies based on the causative organism, valve involvement, and promptness of treatment, with bacterial endocarditis often requiring extended antibiotic therapy and sometimes surgery to prevent severe heart damage or embolic events. Septicemia outcomes depend on early recognition and management of the systemic infection, as delayed treatment can lead to septic shock, multi-organ failure, and high mortality rates. Both conditions demand aggressive care, but endocarditis generally has a more prolonged clinical course, while septicemia requires immediate intervention to improve survival chances.
Prevention and Patient Education
Prevention of endocarditis centers on maintaining good oral hygiene and antibiotic prophylaxis before certain dental or surgical procedures, especially in patients with predisposing heart conditions. Septicemia prevention emphasizes prompt treatment of infections, proper wound care, and sterile techniques in medical settings to avoid bloodstream infections. Patient education should highlight recognizing early symptoms, adherence to prescribed antimicrobial regimens, and the importance of regular medical follow-up to reduce complications associated with both conditions.
Endocarditis Infographic
 libterm.com
libterm.com