Hirsutism and hypertrichosis both involve excessive hair growth but differ in cause and pattern; hirsutism refers to androgen-dependent hair growth typically in women, while hypertrichosis is characterized by abnormal hair growth anywhere on the body, independent of hormonal influence. Understanding these distinctions is crucial for accurate diagnosis and effective treatment plans. Explore the full article to learn how these conditions affect your health and what options are available for management.
Table of Comparison
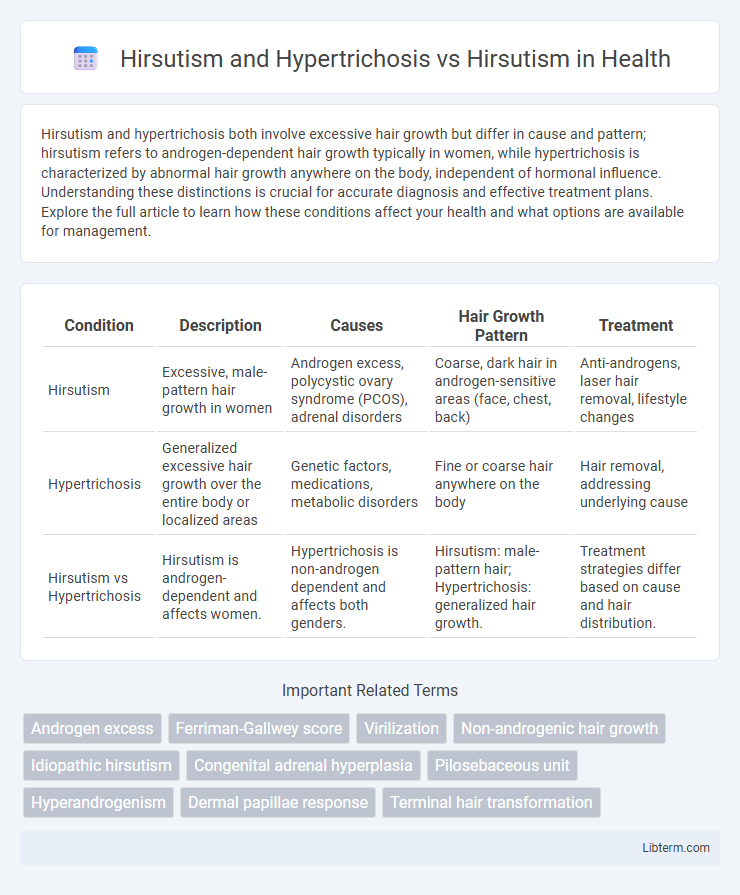
| Condition | Description | Causes | Hair Growth Pattern | Treatment |
|---|---|---|---|---|
| Hirsutism | Excessive, male-pattern hair growth in women | Androgen excess, polycystic ovary syndrome (PCOS), adrenal disorders | Coarse, dark hair in androgen-sensitive areas (face, chest, back) | Anti-androgens, laser hair removal, lifestyle changes |
| Hypertrichosis | Generalized excessive hair growth over the entire body or localized areas | Genetic factors, medications, metabolic disorders | Fine or coarse hair anywhere on the body | Hair removal, addressing underlying cause |
| Hirsutism vs Hypertrichosis | Hirsutism is androgen-dependent and affects women. | Hypertrichosis is non-androgen dependent and affects both genders. | Hirsutism: male-pattern hair; Hypertrichosis: generalized hair growth. | Treatment strategies differ based on cause and hair distribution. |
Understanding Hirsutism: Definition and Causes
Hirsutism is characterized by excessive, male-pattern hair growth in women, primarily caused by elevated androgen levels or increased sensitivity of hair follicles to these hormones, often linked to conditions such as polycystic ovary syndrome (PCOS) and adrenal hyperplasia. Hypertrichosis involves generalized excessive hair growth unrelated to androgen levels, affecting both men and women, and can be congenital or acquired due to factors like medications or metabolic disorders. Understanding the distinct etiologies of hirsutism and hypertrichosis is essential for accurate diagnosis and targeted treatment strategies.
What is Hypertrichosis? Key Differences from Hirsutism
Hypertrichosis is a condition characterized by excessive hair growth on any part of the body, independent of androgen levels, whereas hirsutism specifically refers to excessive terminal hair growth in women following a male-pattern distribution due to elevated androgens. Hypertrichosis can be congenital or acquired and affects both genders, with hair growth possibly covering the entire body or localized areas. Key differences include the causes, distribution patterns, and hormonal involvement, with hypertrichosis not linked to androgen excess, unlike hirsutism which results from hormonal imbalances such as polycystic ovary syndrome (PCOS) or adrenal disorders.
Comparing Hirsutism and Hypertrichosis: Clinical Features
Hirsutism is characterized by excessive terminal hair growth in androgen-dependent areas of women, typically following a male-pattern distribution on the face, chest, and back, driven by androgen excess. Hypertrichosis involves generalized or localized excessive hair growth that affects areas not usually androgen-sensitive and can occur in both genders, independent of hormonal influence. Clinically, hirsutism signifies endocrine or metabolic disorders such as polycystic ovary syndrome, whereas hypertrichosis often results from genetic factors, medications, or systemic diseases without androgen correlation.
Hormonal Imbalance in Hirsutism: Pathophysiology
Hormonal imbalance in hirsutism primarily involves excess androgen production or heightened skin sensitivity to androgens, leading to the growth of coarse, dark terminal hairs in a male-pattern distribution. Hirsutism differs from hypertrichosis, which is characterized by generalized, non-androgen-dependent excessive hair growth that lacks this specific hormonal etiology. The pathophysiology of hirsutism often traces back to conditions such as polycystic ovary syndrome (PCOS), adrenal hyperplasia, or androgen-secreting tumors causing elevated testosterone and DHEA-S levels.
Genetic and Non-Hormonal Triggers of Hypertrichosis
Hirsutism typically results from androgen excess causing excessive terminal hair growth in women, whereas hypertrichosis involves generalized hair growth due to genetic or non-hormonal factors independent of androgen levels. Genetic triggers of hypertrichosis include congenital syndromes such as Ambras syndrome and congenital hypertrichosis lanuginosa, characterized by abnormal hair follicle regulation. Non-hormonal causes encompass drug-induced hypertrichosis from medications like minoxidil and phenytoin, as well as systemic conditions such as porphyria, all leading to excessive hair growth without androgenic involvement.
Diagnostic Criteria: How to Identify Each Condition
Hirsutism is characterized by excessive terminal hair growth in women following a male-pattern distribution, primarily evaluated using the Ferriman-Gallwey scoring system to assess hair density in androgen-sensitive areas. Hypertrichosis involves generalized or localized excessive hair growth irrespective of androgen influence, detectable through clinical examination distinguishing it from androgen-dependent patterns. Diagnostic criteria for hirsutism focus on hormonal assays measuring serum testosterone and androgen levels, while hypertrichosis diagnosis relies on identifying non-androgenic causes such as genetic factors, medications, or systemic diseases.
Assessment Tools: Hirsutism vs Hypertrichosis Evaluation
Assessment tools for hirsutism primarily involve the Ferriman-Gallwey scoring system, which quantitatively evaluates terminal hair growth in androgen-sensitive areas to determine severity. Hypertrichosis evaluation relies on clinical examination and patient history to differentiate the generalized or localized excessive hair growth unrelated to androgen levels. Distinguishing hirsutism from hypertrichosis through these targeted assessment methods guides accurate diagnosis and appropriate treatment planning.
Treatment Approaches: Hirsutism versus Hypertrichosis
Treatment approaches for hirsutism primarily target androgen excess and often include anti-androgen medications like spironolactone, oral contraceptives, and lifestyle modifications to manage hormonal imbalances. Hypertrichosis treatment focuses more on cosmetic methods such as laser hair removal, electrolysis, and topical depilatories, as it is usually unrelated to hormonal abnormalities. Understanding the underlying cause distinguishes therapeutic strategies, with hirsutism requiring endocrine evaluation while hypertrichosis often responds to physical hair reduction techniques.
Psychological and Social Impact of Excess Hair Growth
Excess hair growth in hirsutism and hypertrichosis often leads to significant psychological distress, including low self-esteem and anxiety, due to societal beauty norms and gender expectations. Women with hirsutism experience stigma that can result in social withdrawal, depression, and impaired interpersonal relationships. Unlike hypertrichosis, which affects hair growth more diffusely, hirsutism predominantly impacts androgen-sensitive areas, intensifying its social and emotional consequences.
Prognosis and Long-term Management Strategies
Hirsutism and hypertrichosis differ significantly in prognosis and long-term management, with hirsutism often linked to androgen excess disorders requiring hormonal regulation and lifestyle modifications. Hypertrichosis, characterized by excessive hair growth independent of androgen levels, typically has a stable prognosis but may necessitate cosmetic or dermatological interventions. Long-term management of hirsutism centers on addressing underlying endocrine abnormalities, using medications like anti-androgens or oral contraceptives, while hypertrichosis management emphasizes hair removal techniques and monitoring for associated systemic conditions.
Hirsutism and Hypertrichosis Infographic
 libterm.com
libterm.com