Osteoarthritis is a common degenerative joint disease characterized by the breakdown of cartilage, leading to pain, stiffness, and reduced mobility. Effective management includes physical therapy, medications, and lifestyle changes aimed at reducing symptoms and improving joint function. Discover how you can better understand and manage osteoarthritis by exploring the detailed information in the rest of this article.
Table of Comparison
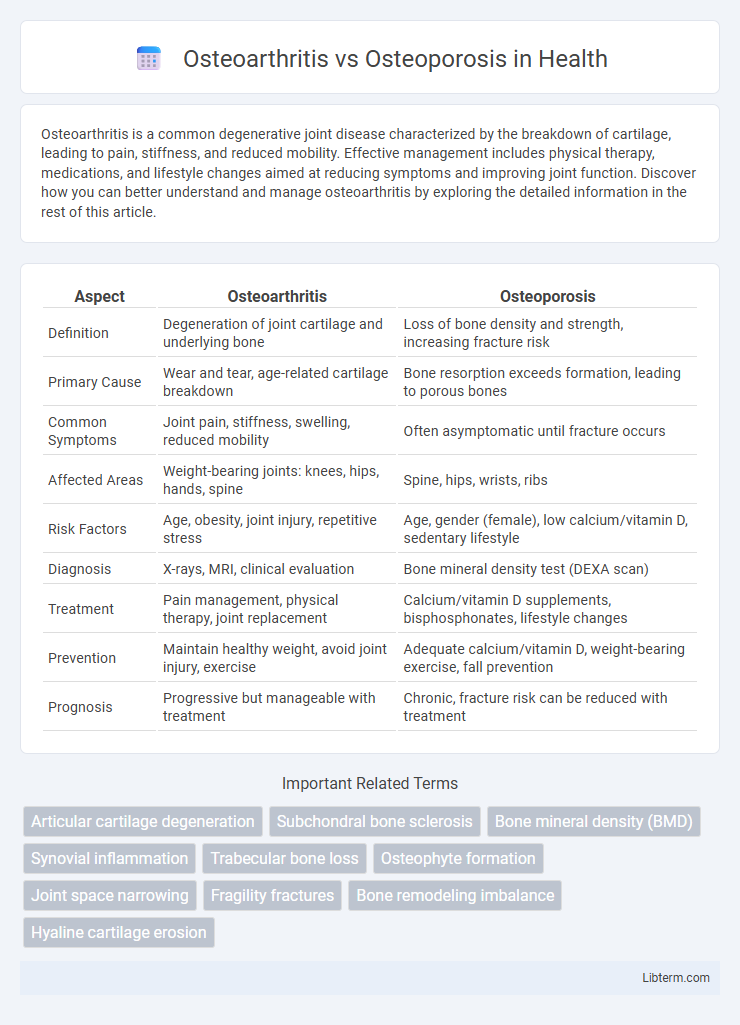
| Aspect | Osteoarthritis | Osteoporosis |
|---|---|---|
| Definition | Degeneration of joint cartilage and underlying bone | Loss of bone density and strength, increasing fracture risk |
| Primary Cause | Wear and tear, age-related cartilage breakdown | Bone resorption exceeds formation, leading to porous bones |
| Common Symptoms | Joint pain, stiffness, swelling, reduced mobility | Often asymptomatic until fracture occurs |
| Affected Areas | Weight-bearing joints: knees, hips, hands, spine | Spine, hips, wrists, ribs |
| Risk Factors | Age, obesity, joint injury, repetitive stress | Age, gender (female), low calcium/vitamin D, sedentary lifestyle |
| Diagnosis | X-rays, MRI, clinical evaluation | Bone mineral density test (DEXA scan) |
| Treatment | Pain management, physical therapy, joint replacement | Calcium/vitamin D supplements, bisphosphonates, lifestyle changes |
| Prevention | Maintain healthy weight, avoid joint injury, exercise | Adequate calcium/vitamin D, weight-bearing exercise, fall prevention |
| Prognosis | Progressive but manageable with treatment | Chronic, fracture risk can be reduced with treatment |
Introduction to Osteoarthritis and Osteoporosis
Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage and underlying bone, leading to pain and stiffness primarily in the knees, hips, and hands. Osteoporosis is a bone disease marked by decreased bone density and increased fracture risk, often affecting the spine, hips, and wrists. Both conditions commonly occur in older adults but differ fundamentally in their impact on joint function versus bone strength.
Defining Osteoarthritis: Causes and Risk Factors
Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage, leading to pain, stiffness, and reduced mobility in affected joints. Causes include aging, joint injury, repetitive stress, and genetic predisposition, while risk factors encompass obesity, gender (more common in women), and occupations involving heavy physical labor. Unlike osteoporosis, which affects bone density, osteoarthritis primarily impacts joint cartilage and connective tissues.
Understanding Osteoporosis: Causes and Risk Factors
Osteoporosis is a bone disease characterized by decreased bone density and increased fracture risk, primarily caused by aging, hormonal changes such as reduced estrogen levels in postmenopausal women, and inadequate calcium and vitamin D intake. Genetic factors, sedentary lifestyle, smoking, excessive alcohol consumption, and certain medications like corticosteroids also contribute to weakened bone structure. Unlike osteoarthritis, which affects joint cartilage and causes pain and stiffness, osteoporosis primarily compromises bone strength without directly affecting joints.
Key Differences Between Osteoarthritis and Osteoporosis
Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage, causing joint pain and stiffness primarily in weight-bearing joints like knees and hips, while osteoporosis is a metabolic bone disorder marked by decreased bone density and increased fracture risk, often affecting the spine, hips, and wrists. Unlike osteoarthritis, which affects joint function and mobility, osteoporosis primarily weakens bone structure without direct joint involvement. Diagnostic methods differ, with osteoarthritis confirmed via joint X-rays showing cartilage loss and osteophytes, whereas osteoporosis is diagnosed through bone mineral density tests such as DEXA scans.
Signs and Symptoms of Osteoarthritis
Osteoarthritis primarily manifests through joint pain, stiffness, and reduced mobility, affecting weight-bearing joints such as the knees, hips, and spine. Unlike osteoporosis, which is characterized by bone density loss and increased fracture risk without early symptoms, osteoarthritis involves cartilage degeneration leading to swelling, tenderness, and crepitus during joint movement. Common signs include morning stiffness lasting less than 30 minutes and joint deformities in advanced stages.
Signs and Symptoms of Osteoporosis
Osteoporosis primarily manifests through signs such as decreased bone density, resulting in fragile bones that fracture easily, often with minimal trauma. Common symptoms include back pain caused by vertebral fractures, loss of height over time, and a stooped posture due to spinal compression. Unlike osteoarthritis, which presents joint pain and stiffness, osteoporosis is often symptomless until a fracture occurs, making early diagnosis critical.
Diagnostic Methods for Osteoarthritis vs Osteoporosis
Osteoarthritis diagnosis primarily relies on clinical evaluation, patient history, and imaging techniques such as X-rays to detect joint space narrowing, osteophyte formation, and subchondral sclerosis. Osteoporosis is diagnosed using bone mineral density (BMD) measurement through dual-energy X-ray absorptiometry (DEXA) scans, which quantify bone loss and fracture risk. While blood tests and markers of bone turnover assist osteoporosis assessment, these are less relevant for osteoarthritis diagnosis, emphasizing distinct diagnostic pathways for these conditions.
Treatment Options for Osteoarthritis and Osteoporosis
Treatment options for osteoarthritis primarily include pain management through nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy to improve joint function, and in severe cases, joint replacement surgery. Osteoporosis treatment focuses on bone density preservation using bisphosphonates, calcium and vitamin D supplementation, and lifestyle changes such as weight-bearing exercises to reduce fracture risk. Both conditions benefit from early diagnosis and personalized management plans to improve quality of life and prevent complications.
Prevention Strategies for Bone and Joint Health
Osteoarthritis prevention centers on maintaining joint mobility through regular low-impact exercise and weight management to reduce stress on cartilage. Osteoporosis prevention emphasizes adequate calcium and vitamin D intake, along with resistance training to enhance bone density and strength. Both conditions benefit from lifestyle choices that support musculoskeletal health, including avoiding smoking and excessive alcohol consumption.
Living with Osteoarthritis or Osteoporosis: Tips for Improved Quality of Life
Managing osteoarthritis involves regular low-impact exercises like swimming or walking to reduce joint stiffness and maintain flexibility, while using pain relief methods such as OTC NSAIDs or physical therapy enhances daily comfort. Living with osteoporosis requires a diet rich in calcium and vitamin D, weight-bearing exercises to strengthen bones, and fall prevention strategies to avoid fractures. Both conditions benefit from lifestyle adjustments, including maintaining a healthy weight, avoiding smoking, and regular medical monitoring to optimize quality of life.
Osteoarthritis Infographic
 libterm.com
libterm.com