Endogenous refers to processes or factors that originate from within a system, organism, or cell, playing a crucial role in biological and ecological functions. Understanding endogenous mechanisms helps unravel how internal influences shape behavior, growth, or responses without external intervention. Discover how endogenous elements impact your health and environment in the rest of this article.
Table of Comparison
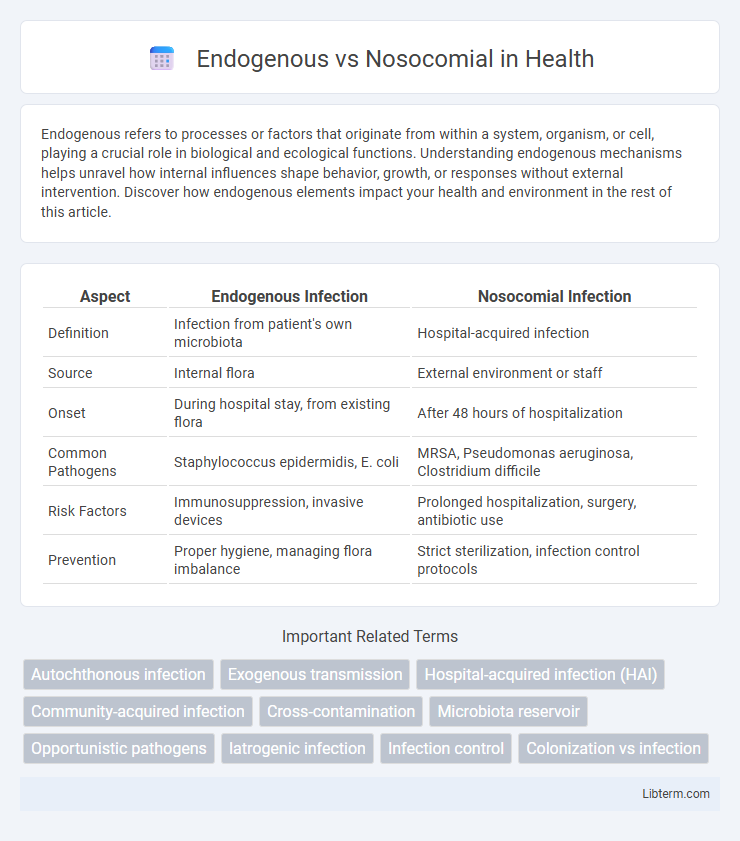
| Aspect | Endogenous Infection | Nosocomial Infection |
|---|---|---|
| Definition | Infection from patient's own microbiota | Hospital-acquired infection |
| Source | Internal flora | External environment or staff |
| Onset | During hospital stay, from existing flora | After 48 hours of hospitalization |
| Common Pathogens | Staphylococcus epidermidis, E. coli | MRSA, Pseudomonas aeruginosa, Clostridium difficile |
| Risk Factors | Immunosuppression, invasive devices | Prolonged hospitalization, surgery, antibiotic use |
| Prevention | Proper hygiene, managing flora imbalance | Strict sterilization, infection control protocols |
Introduction to Infections: Endogenous vs Nosocomial
Endogenous infections originate from the patient's own microbiota, often triggered by an imbalance or immune suppression, whereas nosocomial infections are acquired within healthcare settings, typically caused by external pathogens. Understanding the distinction between endogenous and nosocomial infections is critical for effective infection control, as endogenous infections demand strategies targeting host factors, while nosocomial infections require robust environmental and procedural hygiene protocols. Key pathogens in nosocomial infections include multi-drug-resistant organisms like MRSA and Clostridium difficile, highlighting the importance of surveillance and antimicrobial stewardship in hospital environments.
Defining Endogenous Infections
Endogenous infections arise from the patient's own microbiota when altered by factors such as antibiotic use or immune suppression. These infections occur when normally harmless microorganisms become opportunistic pathogens within the host, leading to diseases like urinary tract infections or bloodstream infections. Understanding the endogenous source is crucial for targeted treatment and prevention strategies distinct from nosocomial infections originating from the hospital environment.
What Are Nosocomial Infections?
Nosocomial infections, also known as hospital-acquired infections (HAIs), occur during a patient's stay in a hospital or healthcare facility and were neither present nor incubating at the time of admission. These infections commonly involve pathogens such as Staphylococcus aureus, including MRSA, Clostridium difficile, and various multidrug-resistant organisms. Understanding the distinction between endogenous infections, caused by the patient's own microbiota, and nosocomial infections, which are acquired from the hospital environment, is crucial for infection control and prevention strategies.
Key Differences Between Endogenous and Nosocomial Infections
Endogenous infections originate from the patient's own microbiota, whereas nosocomial infections are acquired within a healthcare setting. Endogenous infections often result from opportunistic pathogens triggered by immune suppression or invasive procedures, while nosocomial infections involve external sources such as contaminated equipment or hospital personnel. Key differences include the infection source, with endogenous infections arising internally, and nosocomial infections caused by external factors specific to healthcare environments.
Common Causes of Endogenous Infections
Endogenous infections arise from the patient's own microbiota when normally harmless organisms become pathogenic due to immune suppression, surgery, or disruption of natural barriers, commonly caused by bacteria such as Staphylococcus aureus, Escherichia coli, and Candida species. These infections frequently occur in immunocompromised individuals or those undergoing invasive procedures, where the balance of the microbiome is disturbed. Nosocomial infections, in contrast, are hospital-acquired and often involve multidrug-resistant pathogens introduced from external sources.
Major Sources of Nosocomial Infections
Major sources of nosocomial infections include contaminated medical devices, healthcare personnel, and hospital environments such as surfaces and air systems. Pathogens such as Staphylococcus aureus, Pseudomonas aeruginosa, and Clostridium difficile often originate from these reservoirs, leading to infections like bloodstream infections, surgical site infections, and ventilator-associated pneumonia. Proper sterilization, hand hygiene, and environmental cleaning are critical to controlling these exogenous sources of hospital-acquired infections.
Risk Factors Involved in Both Infection Types
Endogenous infections arise from the patient's own microbiota due to factors like immunosuppression, breaches in skin or mucosal barriers, and underlying chronic diseases, which disrupt normal microbial balance. Nosocomial infections, acquired within healthcare settings, are influenced by risk factors such as invasive procedures, prolonged hospitalization, use of indwelling devices, and exposure to multidrug-resistant organisms. Both infection types share contributors like impaired host defenses and antibiotic usage, but nosocomial infections uniquely involve environmental contamination and cross-transmission from healthcare workers or equipment.
Diagnosis and Detection Methods
Endogenous infections originate from the patient's own microbiota, requiring diagnostic methods such as molecular typing and genetic sequencing to differentiate from exogenous sources. Nosocomial infections, acquired in healthcare settings, are primarily detected through culture-based techniques, antimicrobial susceptibility testing, and epidemiological surveillance. Advanced rapid diagnostic tools, including PCR and MALDI-TOF mass spectrometry, enhance the accuracy and speed of identifying both infection types.
Preventive Strategies for Each Infection
Preventive strategies for endogenous infections emphasize maintaining a patient's natural defenses through proper hygiene, nutritional support, and minimizing invasive procedures to reduce microbial translocation from the host's own flora. Nosocomial infections require rigorous infection control measures such as sterilization of medical equipment, hand hygiene protocols, isolation procedures, and timely use of antibiotics guided by antimicrobial stewardship programs to prevent pathogen transmission within healthcare settings. Targeted surveillance and education of healthcare personnel are critical components in reducing the incidence of both endogenous and nosocomial infections.
Conclusion: Choosing Effective Infection Control Measures
Effective infection control measures must distinguish between endogenous and nosocomial infections to tailor prevention strategies accurately. Endogenous infections arise from a patient's own microbiota, requiring interventions that enhance immunity and maintain healthy flora, while nosocomial infections originate from the hospital environment, necessitating strict hygiene protocols and environmental decontamination. Prioritizing targeted surveillance, hand hygiene, and antimicrobial stewardship optimizes patient outcomes and minimizes infection rates in healthcare settings.
Endogenous Infographic
 libterm.com
libterm.com