Hypoxemia occurs when your blood oxygen levels fall below normal, leading to symptoms such as shortness of breath, rapid heartbeat, and confusion. Causes range from respiratory conditions like COPD and asthma to high altitudes or heart problems. Explore the rest of the article to understand hypoxemia's causes, symptoms, and possible treatments.
Table of Comparison
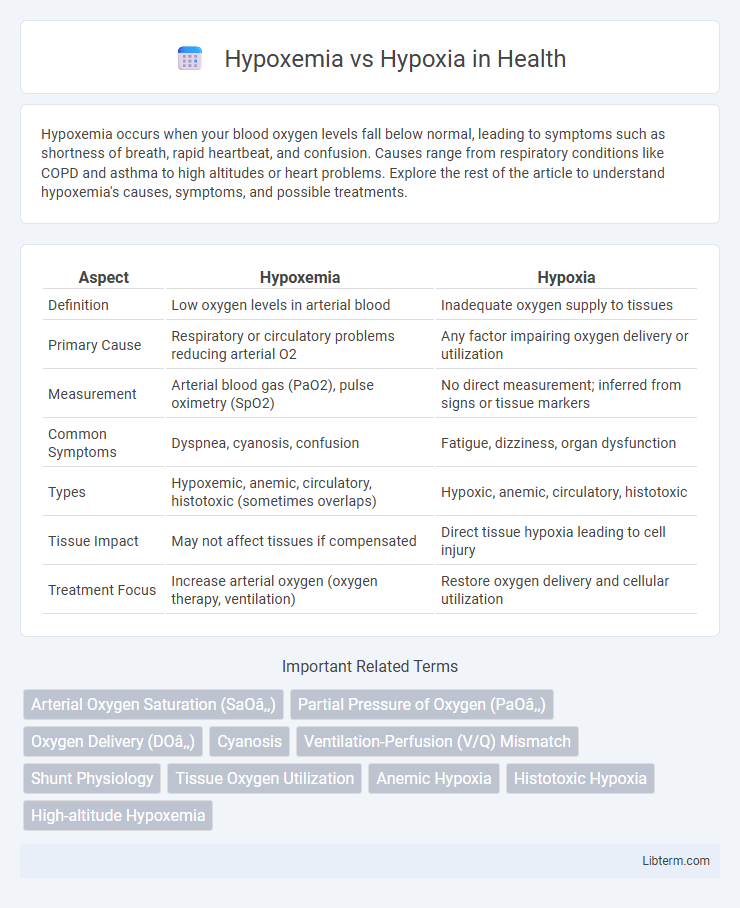
| Aspect | Hypoxemia | Hypoxia |
|---|---|---|
| Definition | Low oxygen levels in arterial blood | Inadequate oxygen supply to tissues |
| Primary Cause | Respiratory or circulatory problems reducing arterial O2 | Any factor impairing oxygen delivery or utilization |
| Measurement | Arterial blood gas (PaO2), pulse oximetry (SpO2) | No direct measurement; inferred from signs or tissue markers |
| Common Symptoms | Dyspnea, cyanosis, confusion | Fatigue, dizziness, organ dysfunction |
| Types | Hypoxemic, anemic, circulatory, histotoxic (sometimes overlaps) | Hypoxic, anemic, circulatory, histotoxic |
| Tissue Impact | May not affect tissues if compensated | Direct tissue hypoxia leading to cell injury |
| Treatment Focus | Increase arterial oxygen (oxygen therapy, ventilation) | Restore oxygen delivery and cellular utilization |
Understanding Hypoxemia and Hypoxia
Hypoxemia refers to low oxygen levels specifically in the blood, measured by arterial oxygen tension (PaO2) below 80 mmHg or oxygen saturation (SpO2) under 90%, while hypoxia describes insufficient oxygen supply at the tissue level. Understanding hypoxemia involves evaluating causes such as impaired gas exchange, ventilation-perfusion mismatch, or diffusion defects, whereas hypoxia can result from hypoxemia or other factors like anemia or circulatory failure. Accurate diagnosis requires arterial blood gas analysis for hypoxemia and clinical assessment of organ function to identify hypoxia.
Key Differences Between Hypoxemia and Hypoxia
Hypoxemia refers specifically to low oxygen levels in the blood, typically measured by arterial oxygen saturation below 90%, whereas hypoxia describes inadequate oxygen supply to tissues despite adequate blood oxygen levels. Hypoxemia is usually detected through pulse oximetry or arterial blood gas analysis, while hypoxia is assessed by clinical signs or tissue oxygenation studies. Understanding these distinctions aids accurate diagnosis and targeted treatment in respiratory and circulatory disorders.
Causes of Hypoxemia
Hypoxemia is primarily caused by factors such as ventilation-perfusion mismatch, diffusion impairment, hypoventilation, and reduced inspired oxygen levels, leading to decreased arterial oxygen tension. Lung diseases like chronic obstructive pulmonary disease (COPD), pneumonia, pulmonary edema, and pulmonary embolism frequently contribute to hypoxemia by disrupting oxygen transfer in the lungs. Understanding these causes is crucial for differentiating hypoxemia from hypoxia, which involves inadequate oxygen supply at the tissue level despite normal arterial oxygenation.
Causes of Hypoxia
Hypoxia occurs when tissues are deprived of adequate oxygen supply due to causes such as respiratory disorders like chronic obstructive pulmonary disease (COPD), anemia reducing oxygen-carrying capacity, or circulatory issues including shock and heart failure. Environmental factors like high altitude can also induce hypoxia by lowering atmospheric oxygen pressure. Understanding these causes is crucial for distinguishing hypoxia from hypoxemia, which specifically refers to low oxygen levels in arterial blood.
Signs and Symptoms
Hypoxemia presents with signs such as cyanosis, tachypnea, and low oxygen saturation levels measured by pulse oximetry, indicating reduced oxygen in arterial blood. Hypoxia symptoms include confusion, headache, tachycardia, and impaired coordination due to insufficient oxygen supply to tissues despite normal oxygen levels in the blood. Both conditions require prompt recognition through clinical evaluation and diagnostic tests like arterial blood gas analysis to prevent organ damage.
Diagnostic Approaches
Hypoxemia is diagnosed primarily through arterial blood gas (ABG) analysis measuring partial pressure of oxygen (PaO2) and oxygen saturation levels, while pulse oximetry provides a non-invasive estimate of blood oxygenation. Hypoxia diagnosis involves assessing clinical signs alongside tools like ABG, pulse oximetry, and imaging studies such as chest X-rays or CT scans to identify underlying causes affecting tissue oxygen delivery. Advanced diagnostics may include pulmonary function tests and cardiac evaluations to distinguish hypoxemia-induced hypoxia from other etiologies.
Risk Factors and Common Conditions
Hypoxemia is characterized by low oxygen levels in the blood, often caused by risk factors such as chronic obstructive pulmonary disease (COPD), pneumonia, and pulmonary embolism, leading to impaired oxygen exchange in the lungs. Hypoxia refers to inadequate oxygen supply to tissues despite normal blood oxygen levels, commonly associated with conditions like anemia, heart failure, and carbon monoxide poisoning. Both conditions share overlapping risk factors like high altitudes and respiratory disorders, but their clinical manifestations and treatment approaches differ significantly.
Treatment and Management Options
Treatment of hypoxemia primarily involves oxygen therapy through nasal cannula, face mask, or mechanical ventilation to restore adequate blood oxygen levels. Management of hypoxia requires addressing the underlying cause, such as improving tissue perfusion in shock or correcting anemia with blood transfusions. Both conditions may benefit from supportive care including medications to optimize cardiovascular function and ensure proper oxygen delivery to tissues.
Prevention Strategies
Preventing hypoxemia involves ensuring adequate oxygen delivery through strategies such as using supplemental oxygen therapy for patients with respiratory disorders and maintaining airway patency. Hypoxia prevention focuses on optimizing tissue oxygenation by monitoring hemoglobin levels, enhancing cardiovascular health, and avoiding conditions that impair oxygen utilization at the cellular level. Early detection of risk factors like chronic obstructive pulmonary disease (COPD) or anemia is crucial for implementing effective prevention protocols.
Frequently Asked Questions (FAQs)
Hypoxemia refers to low oxygen levels in the blood, whereas hypoxia indicates insufficient oxygen supply to the tissues despite normal blood oxygen levels. Common FAQs address causes of hypoxemia such as respiratory illnesses, differences between hypoxemia and hypoxia symptoms, diagnostic methods like pulse oximetry and arterial blood gas analysis, and treatment options including supplemental oxygen therapy. Understanding these distinctions helps guide accurate diagnosis and effective management of oxygen deficiency-related conditions.
Hypoxemia Infographic
 libterm.com
libterm.com