Coagulation is a critical process in blood clotting where blood changes from a liquid to a gel, forming a clot to prevent excessive bleeding. Understanding the mechanisms behind coagulation can help you recognize disorders related to clotting, such as hemophilia or deep vein thrombosis. Explore the rest of the article to learn how coagulation impacts your health and the latest treatments available.
Table of Comparison
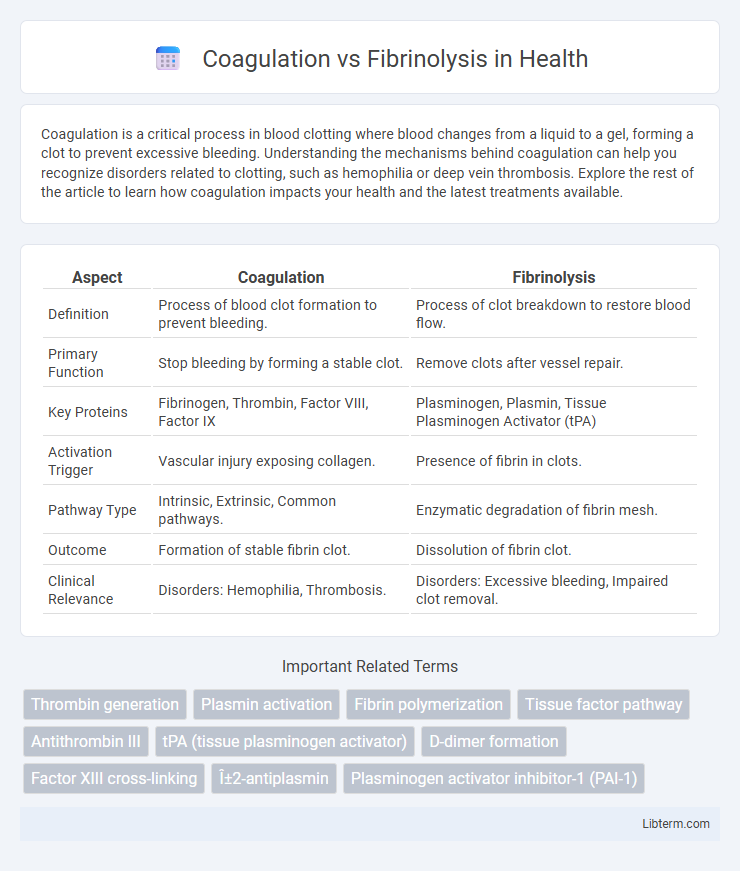
| Aspect | Coagulation | Fibrinolysis |
|---|---|---|
| Definition | Process of blood clot formation to prevent bleeding. | Process of clot breakdown to restore blood flow. |
| Primary Function | Stop bleeding by forming a stable clot. | Remove clots after vessel repair. |
| Key Proteins | Fibrinogen, Thrombin, Factor VIII, Factor IX | Plasminogen, Plasmin, Tissue Plasminogen Activator (tPA) |
| Activation Trigger | Vascular injury exposing collagen. | Presence of fibrin in clots. |
| Pathway Type | Intrinsic, Extrinsic, Common pathways. | Enzymatic degradation of fibrin mesh. |
| Outcome | Formation of stable fibrin clot. | Dissolution of fibrin clot. |
| Clinical Relevance | Disorders: Hemophilia, Thrombosis. | Disorders: Excessive bleeding, Impaired clot removal. |
Introduction to Hemostasis: Coagulation and Fibrinolysis
Hemostasis is a critical physiological process involving coagulation and fibrinolysis that maintains blood fluidity and prevents excessive bleeding. Coagulation is the cascade of enzymatic reactions leading to the formation of a stable fibrin clot, while fibrinolysis breaks down clots to restore normal blood flow. The balance between these two systems is essential for vascular integrity and preventing thrombotic or hemorrhagic disorders.
The Physiology of Blood Coagulation
Blood coagulation is a complex physiological process involving the activation of clotting factors that convert fibrinogen into a stable fibrin mesh, essential for hemostasis. Platelets play a crucial role by adhering to the damaged endothelium and releasing pro-coagulant substances that amplify the coagulation cascade. The balance between coagulation and fibrinolysis maintains vascular integrity, preventing excessive bleeding while avoiding thrombosis.
Key Factors and Pathways in Coagulation
Coagulation involves a complex cascade primarily driven by clotting factors such as Factor VIII, Factor IX, and Factor X, which activate thrombin to convert fibrinogen into fibrin, forming a stable blood clot. The intrinsic and extrinsic pathways converge at the activation of Factor X, initiating the common pathway essential for clot formation. Key regulatory proteins like tissue factor and platelets coordinate this process, ensuring effective hemostasis while balancing procoagulant and anticoagulant forces.
Overview of the Fibrinolytic System
The fibrinolytic system is a crucial biological process responsible for breaking down fibrin clots, ensuring vascular patency and preventing thrombosis. Key components include plasminogen, tissue plasminogen activator (tPA), and plasmin, which collectively degrade fibrin into soluble fragments. This system operates in balance with coagulation pathways to regulate hemostasis and maintain blood flow.
Major Regulators of Fibrinolysis
Major regulators of fibrinolysis include tissue plasminogen activator (tPA), which initiates the conversion of plasminogen to plasmin to dissolve fibrin clots. Plasminogen activator inhibitor-1 (PAI-1) serves as a primary inhibitor of tPA, controlling the balance between clot breakdown and formation. Alpha-2-antiplasmin directly inhibits plasmin activity, preventing excessive fibrinolysis and maintaining hemostatic equilibrium.
Coagulation vs Fibrinolysis: Key Differences
Coagulation is the physiological process that forms blood clots to prevent excessive bleeding by activating platelets and fibrin networks, while fibrinolysis breaks down clots to restore normal blood flow by degrading fibrin through plasmin activation. The key difference lies in their opposing roles: coagulation promotes clot formation via clotting factors like thrombin, whereas fibrinolysis dissolves clots using enzymes such as plasminogen activators. Balancing coagulation and fibrinolysis is crucial for maintaining hemostasis and preventing disorders like thrombosis or hemorrhage.
Clinical Significance of Coagulation and Fibrinolysis Balance
The clinical significance of maintaining a balance between coagulation and fibrinolysis is critical for preventing pathological conditions such as thrombosis and hemorrhage. Dysregulation can lead to excessive clot formation, increasing the risk of stroke, myocardial infarction, and deep vein thrombosis, while insufficient coagulation or excessive fibrinolysis can cause severe bleeding disorders. Understanding this balance aids in effective management of anticoagulant and thrombolytic therapies to optimize patient outcomes in cardiovascular and hematologic diseases.
Disorders Related to Coagulation and Fibrinolysis Imbalance
Disorders related to coagulation and fibrinolysis imbalance include thrombosis, characterized by excessive clot formation due to hypercoagulability, and bleeding disorders like hemophilia and von Willebrand disease, where impaired coagulation causes inadequate clotting. Hyperfibrinolysis, resulting in excessive clot breakdown, can lead to severe bleeding complications during surgery or trauma. Deficiencies or dysfunctions in key factors such as plasminogen activators, fibrinogen, or coagulation factors VIII and IX contribute to these imbalances, affecting hemostatic stability.
Diagnostic Tests for Coagulation and Fibrinolysis
Diagnostic tests for coagulation include Prothrombin Time (PT), Activated Partial Thromboplastin Time (aPTT), and Thrombin Time (TT), which assess the clotting ability and identify deficiencies or inhibitors in the coagulation cascade. For fibrinolysis evaluation, D-dimer tests and plasminogen activity assays measure fibrin degradation products and plasmin function, respectively, aiding in the detection of excessive clot breakdown or thrombotic disorders. Combining these tests provides a comprehensive assessment of both clot formation and dissolution processes crucial for diagnosing hemostatic imbalances.
Therapeutic Approaches Targeting Hemostatic Balance
Therapeutic approaches targeting hemostatic balance focus on modulating coagulation and fibrinolysis pathways to prevent thrombosis or bleeding disorders. Anticoagulants such as direct oral anticoagulants (DOACs) inhibit key coagulation factors like thrombin and factor Xa, while fibrinolytic agents like tissue plasminogen activator (tPA) promote the breakdown of fibrin clots. Emerging therapies aim to fine-tune this balance by targeting regulatory proteins, including plasminogen activator inhibitor-1 (PAI-1) and protein C pathways, to optimize hemostatic control and reduce adverse events.
Coagulation Infographic
 libterm.com
libterm.com