Intrauterine devices (IUDs) are highly effective, long-term contraceptive options inserted directly into the uterus to prevent pregnancy. They work by altering the uterine environment, making it inhospitable for sperm and fertilized eggs. Discover how an intrauterine device might be the right choice for your family planning by reading more in this article.
Table of Comparison
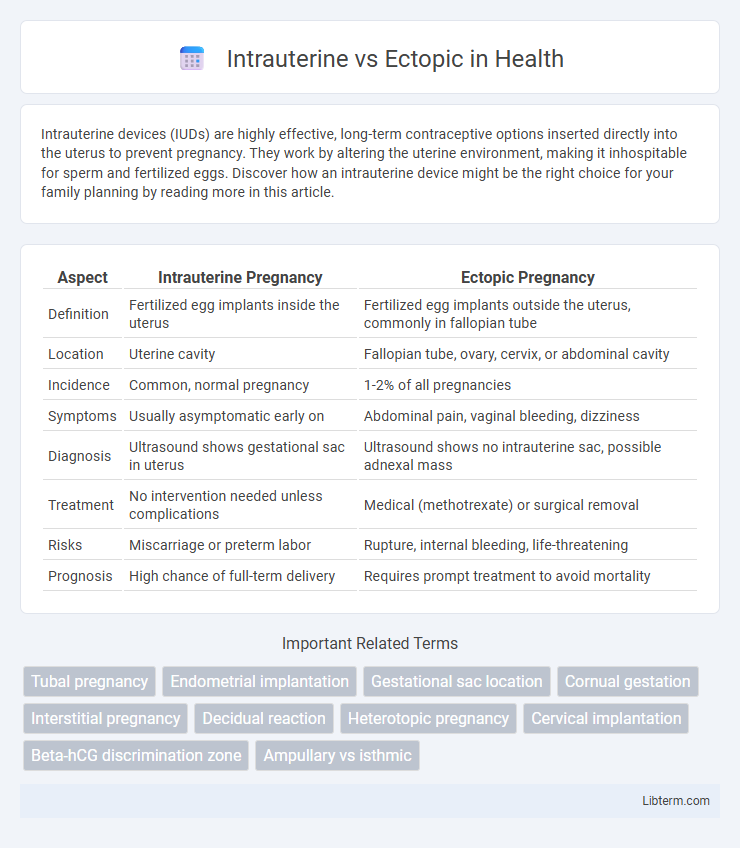
| Aspect | Intrauterine Pregnancy | Ectopic Pregnancy |
|---|---|---|
| Definition | Fertilized egg implants inside the uterus | Fertilized egg implants outside the uterus, commonly in fallopian tube |
| Location | Uterine cavity | Fallopian tube, ovary, cervix, or abdominal cavity |
| Incidence | Common, normal pregnancy | 1-2% of all pregnancies |
| Symptoms | Usually asymptomatic early on | Abdominal pain, vaginal bleeding, dizziness |
| Diagnosis | Ultrasound shows gestational sac in uterus | Ultrasound shows no intrauterine sac, possible adnexal mass |
| Treatment | No intervention needed unless complications | Medical (methotrexate) or surgical removal |
| Risks | Miscarriage or preterm labor | Rupture, internal bleeding, life-threatening |
| Prognosis | High chance of full-term delivery | Requires prompt treatment to avoid mortality |
Understanding Intrauterine and Ectopic Pregnancies
Intrauterine pregnancy occurs when a fertilized egg implants within the uterine cavity, representing a normal and viable pregnancy. Ectopic pregnancy arises when implantation happens outside the uterus, most commonly in the fallopian tubes, posing significant health risks due to potential rupture and hemorrhage. Early diagnosis through ultrasound and serum hCG levels is essential to differentiate between intrauterine and ectopic pregnancies for appropriate medical management.
Key Differences Between Intrauterine and Ectopic Pregnancy
Intrauterine pregnancy occurs when a fertilized egg implants within the uterine cavity, supporting normal fetal development, while ectopic pregnancy happens when implantation takes place outside the uterus, most commonly in the fallopian tubes. Key differences include location, clinical symptoms such as abdominal pain and vaginal bleeding predominantly seen in ectopic cases, and diagnostic methods like transvaginal ultrasound and serum hCG levels that help distinguish between the two. Management strategies vary significantly; intrauterine pregnancies are monitored for normal progression, while ectopic pregnancies require urgent medical or surgical intervention to prevent life-threatening complications.
Causes and Risk Factors of Ectopic Pregnancy
Ectopic pregnancy primarily occurs when a fertilized egg implants outside the uterine cavity, most commonly in the fallopian tubes, due to factors such as previous pelvic infections, tubal surgery, or scarring. Risk factors include a history of pelvic inflammatory disease (PID), endometriosis, previous ectopic pregnancies, and the use of assisted reproductive technologies like IVF. Smoking and age over 35 further increase the likelihood of an ectopic pregnancy by impairing tubal function and embryo transport.
Signs and Symptoms: Intrauterine vs Ectopic
Intrauterine pregnancies typically present with normal signs such as a positive pregnancy test, missed menses, and gradual abdominal growth, often accompanied by mild, manageable discomfort. Ectopic pregnancies commonly exhibit sharp, localized pelvic pain, unilateral to the affected fallopian tube, along with irregular vaginal bleeding and possible shoulder pain due to diaphragmatic irritation from internal bleeding. Early detection relies on ultrasound imaging and monitoring of beta-hCG levels, with severe ectopic cases leading to symptoms of hypovolemic shock requiring urgent medical intervention.
Diagnostic Methods for Pregnancy Location
Transvaginal ultrasound remains the gold standard for distinguishing intrauterine pregnancies from ectopic locations, enabling direct visualization of the gestational sac within the uterus. Quantitative serum beta-hCG levels complement imaging by helping identify abnormal rise patterns suggestive of ectopic implantation when levels do not correspond with ultrasound findings. In ambiguous cases, diagnostic laparoscopy offers definitive localization, especially when non-invasive methods prove inconclusive or when rupture risk exists.
Ultrasound Findings: Intrauterine vs Ectopic
Ultrasound findings for intrauterine pregnancy typically reveal a gestational sac within the endometrial cavity, often with a visible yolk sac or fetal pole confirming viability. In ectopic pregnancy, ultrasound may show an adnexal mass or tubal ring sign, absence of an intrauterine gestational sac, and sometimes free fluid in the pelvis indicating possible rupture. Transvaginal ultrasound is the preferred modality for early detection, offering higher resolution to differentiate between normal intrauterine implantation and ectopic locations.
Treatment Options for Ectopic Pregnancy
Treatment options for ectopic pregnancy primarily include medication with methotrexate, which halts cell growth and dissolves existing cells, suitable for early, unruptured cases. Surgical interventions such as laparoscopy or laparotomy are necessary for ruptured ectopic pregnancies or when methotrexate is contraindicated, aiming to remove the ectopic tissue and preserve fertility. Expectant management may be considered in select stable patients with declining beta-hCG levels, requiring close monitoring to ensure complete resolution.
Management and Care of Intrauterine Pregnancy
Management of intrauterine pregnancy emphasizes regular prenatal care, including routine ultrasounds and monitoring of fetal development to ensure maternal and fetal health. Nutritional guidance, management of pre-existing conditions, and screening for gestational complications like preeclampsia are critical components of care. Early intervention and comprehensive education support optimal pregnancy outcomes and maternal well-being.
Complications and Long-term Outcomes
Intrauterine pregnancies generally have fewer complications compared to ectopic pregnancies, which pose significant risks such as tubal rupture, severe hemorrhage, and infertility. Ectopic pregnancies often require surgical intervention or methotrexate therapy, potentially impacting future fertility and increasing the risk of recurrent ectopic gestations. Long-term outcomes favor intrauterine pregnancies with normal fetal development, while ectopic pregnancies may lead to chronic pelvic pain and compromised reproductive health if not promptly treated.
Prevention, Prognosis, and Patient Counseling
Prevention of ectopic pregnancy involves early prenatal care, managing risk factors such as pelvic inflammatory disease, and avoiding smoking, while intrauterine pregnancies benefit from routine monitoring to ensure proper fetal development. Prognosis for intrauterine pregnancies is generally favorable with timely medical attention, whereas ectopic pregnancies pose significant risks, including tubal rupture and infertility, requiring prompt diagnosis and treatment. Patient counseling emphasizes educating about symptom awareness, importance of early medical evaluation, and potential complications, enabling informed decision-making and improved maternal outcomes.
Intrauterine Infographic
 libterm.com
libterm.com