Leukoplakia is a condition characterized by white patches that form on the mucous membranes of the mouth, often caused by chronic irritation such as tobacco use or alcohol consumption. These patches can sometimes be precancerous, making early detection and monitoring crucial for oral health. Explore the rest of the article to understand the symptoms, causes, and treatment options for leukoplakia to protect your oral well-being.
Table of Comparison
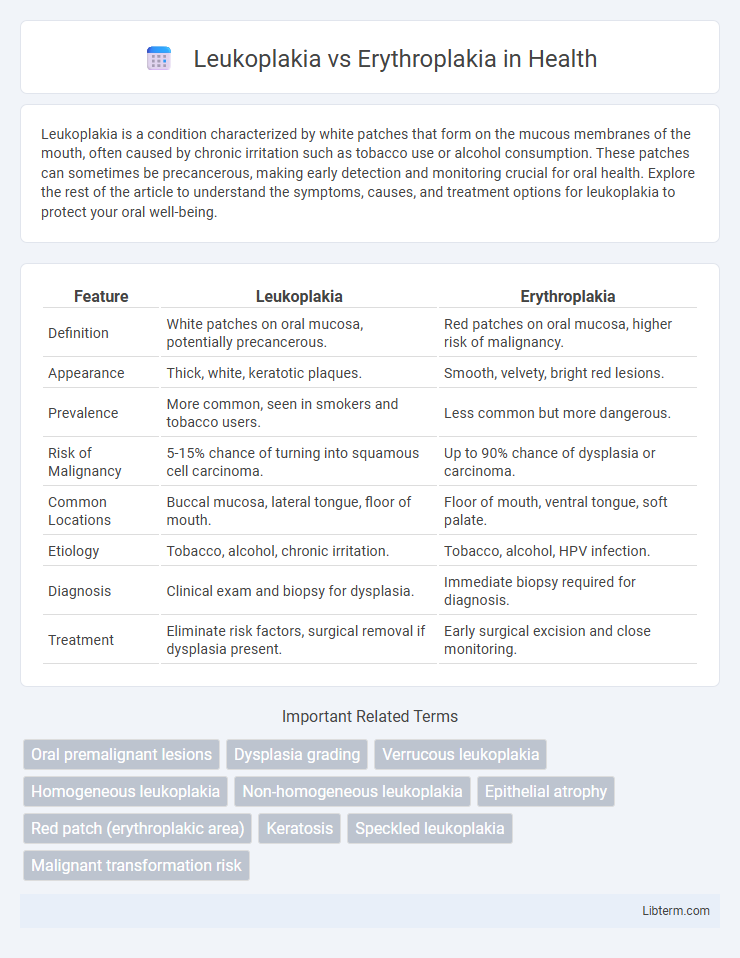
| Feature | Leukoplakia | Erythroplakia |
|---|---|---|
| Definition | White patches on oral mucosa, potentially precancerous. | Red patches on oral mucosa, higher risk of malignancy. |
| Appearance | Thick, white, keratotic plaques. | Smooth, velvety, bright red lesions. |
| Prevalence | More common, seen in smokers and tobacco users. | Less common but more dangerous. |
| Risk of Malignancy | 5-15% chance of turning into squamous cell carcinoma. | Up to 90% chance of dysplasia or carcinoma. |
| Common Locations | Buccal mucosa, lateral tongue, floor of mouth. | Floor of mouth, ventral tongue, soft palate. |
| Etiology | Tobacco, alcohol, chronic irritation. | Tobacco, alcohol, HPV infection. |
| Diagnosis | Clinical exam and biopsy for dysplasia. | Immediate biopsy required for diagnosis. |
| Treatment | Eliminate risk factors, surgical removal if dysplasia present. | Early surgical excision and close monitoring. |
Introduction to Leukoplakia and Erythroplakia
Leukoplakia is a white patch or plaque on the mucous membranes of the oral cavity that cannot be scraped off, often linked to tobacco use and considered a precancerous lesion. Erythroplakia appears as a red, velvety lesion and carries a higher risk for malignant transformation than leukoplakia, frequently associated with dysplasia or carcinoma in situ. Both conditions require careful clinical evaluation and biopsy for accurate diagnosis and management due to their potential progression to oral cancer.
Definition and Clinical Presentation
Leukoplakia presents as white patches on the oral mucosa that cannot be scraped off, often linked to chronic irritation or tobacco use. Erythroplakia manifests as red, velvety lesions on the oral mucosa, with a higher risk of dysplasia or malignancy compared to leukoplakia. Clinically, leukoplakia is typically asymptomatic, while erythroplakia may present with soreness or ulceration, necessitating prompt biopsy for diagnosis.
Epidemiology and Prevalence Rates
Leukoplakia is the most common potentially malignant disorder of the oral mucosa, with a prevalence ranging from 1% to 5% globally, particularly affecting middle-aged and older adults with a higher incidence in tobacco users. Erythroplakia, although less common, presents a prevalence rate of approximately 0.02% to 0.2%, predominantly occurring in males aged 50 to 70 and showing a stronger association with significant dysplasia and malignancy. Both lesions demonstrate higher prevalence in populations with prevalent risk factors such as tobacco smoking, alcohol consumption, and are critical markers for oral cancer screening programs.
Etiological Factors and Risk Contributors
Leukoplakia primarily arises from chronic irritation caused by tobacco use, alcohol consumption, and mechanical trauma, with human papillomavirus (HPV) infections also implicated in its etiology. Erythroplakia, although less common, exhibits a stronger association with heavy smoking and alcohol abuse, showing higher rates of epithelial dysplasia and malignant transformation. Both conditions are influenced by immune suppression and nutritional deficiencies, but erythroplakia carries a significantly higher risk of progressing to squamous cell carcinoma.
Histopathological Features
Leukoplakia typically exhibits hyperkeratosis and epithelial hyperplasia with varying degrees of dysplasia, ranging from mild to severe, but often lacks significant vascular proliferation. In contrast, erythroplakia shows pronounced epithelial dysplasia and often carcinoma in situ, with a thinner epithelial layer and prominent subepithelial vascularization that contributes to its red appearance. These histopathological differences are critical for diagnosis and risk assessment, as erythroplakia generally has a higher malignant transformation potential compared to leukoplakia.
Malignant Transformation Potential
Leukoplakia presents as a white patch on mucous membranes with a malignant transformation rate ranging from 1% to 20%, depending on histopathologic features like dysplasia severity. Erythroplakia, characterized by a red, velvety lesion, carries a significantly higher risk of malignancy, with transformation rates often reported between 30% and 70%. Early biopsy and histological evaluation are critical for both lesions to determine the presence of dysplasia or carcinoma in situ, guiding timely intervention and management.
Diagnostic Methods and Differential Diagnosis
Leukoplakia and erythroplakia are oral mucosal lesions with distinct diagnostic approaches, emphasizing visual inspection, biopsy, and histopathological examination to differentiate benign from potentially malignant changes. Leukoplakia typically presents as a white patch, requiring careful evaluation with toluidine blue staining and brush biopsy to assess dysplasia, whereas erythroplakia appears as a red, velvety lesion with a higher risk of severe dysplasia or carcinoma, often necessitating incisional biopsy for definitive diagnosis. Differential diagnosis includes candidiasis, lichen planus, and traumatic ulcers, highlighting the importance of clinical correlation and microscopic analysis to guide appropriate management.
Management and Treatment Options
Leukoplakia management primarily involves eliminating risk factors such as tobacco and alcohol use, with regular monitoring and biopsy for lesions showing dysplasia. Erythroplakia treatment requires prompt biopsy due to its higher malignant potential, often necessitating surgical excision or laser ablation for confirmed dysplastic or malignant areas. Both conditions benefit from close follow-up to detect and manage any progression to oral cancer.
Prognosis and Patient Outcomes
Leukoplakia generally presents a lower malignant transformation risk compared to erythroplakia, with approximately 3-17% of leukoplakic lesions progressing to oral cancer, while erythroplakia carries a significantly higher risk, with malignant transformation rates ranging from 40-50%. Patient outcomes for leukoplakia are generally favorable with early detection and management, whereas erythroplakia often requires more aggressive intervention due to its association with severe dysplasia or carcinoma in situ. Close monitoring and biopsy are critical for both conditions to improve prognosis and prevent progression to invasive oral squamous cell carcinoma.
Prevention and Surveillance Strategies
Leukoplakia and erythroplakia require rigorous prevention strategies including tobacco cessation, alcohol moderation, and regular oral hygiene to reduce malignant transformation risk. Surveillance involves frequent clinical examinations with biopsy of suspicious lesions, using adjunctive tools like toluidine blue staining or autofluorescence to detect dysplasia early. Early detection through targeted screening programs enhances prognosis by enabling timely intervention in premalignant oral mucosal lesions.
Leukoplakia Infographic
 libterm.com
libterm.com