Hypoxemia occurs when there is an abnormally low concentration of oxygen in the blood, leading to symptoms such as shortness of breath, cyanosis, and confusion. Early detection and treatment are crucial to prevent serious complications like organ damage or respiratory failure. Explore this article to understand the causes, symptoms, and effective management of hypoxemia to protect your health.
Table of Comparison
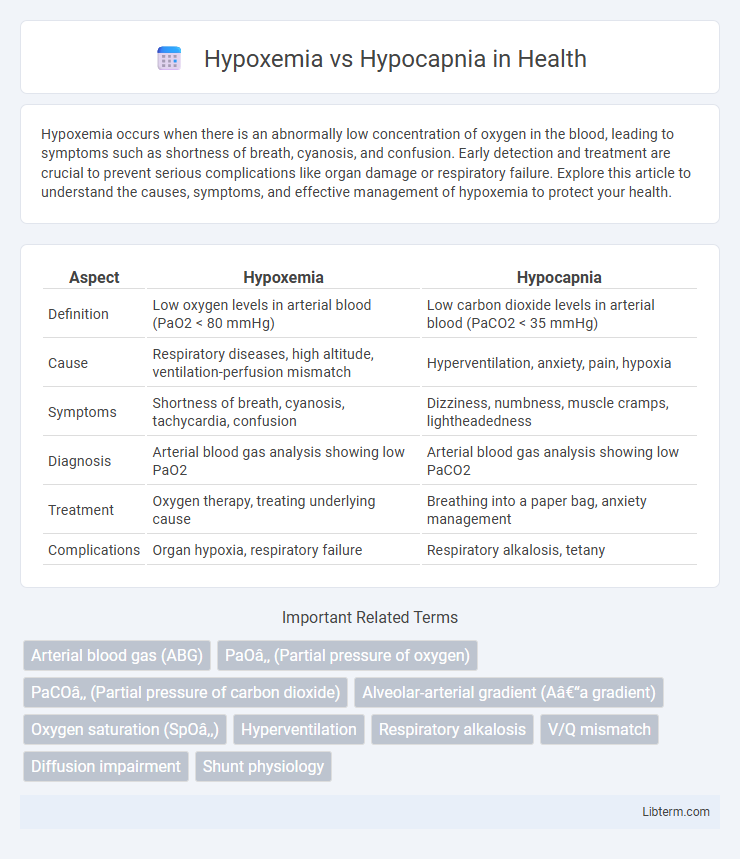
| Aspect | Hypoxemia | Hypocapnia |
|---|---|---|
| Definition | Low oxygen levels in arterial blood (PaO2 < 80 mmHg) | Low carbon dioxide levels in arterial blood (PaCO2 < 35 mmHg) |
| Cause | Respiratory diseases, high altitude, ventilation-perfusion mismatch | Hyperventilation, anxiety, pain, hypoxia |
| Symptoms | Shortness of breath, cyanosis, tachycardia, confusion | Dizziness, numbness, muscle cramps, lightheadedness |
| Diagnosis | Arterial blood gas analysis showing low PaO2 | Arterial blood gas analysis showing low PaCO2 |
| Treatment | Oxygen therapy, treating underlying cause | Breathing into a paper bag, anxiety management |
| Complications | Organ hypoxia, respiratory failure | Respiratory alkalosis, tetany |
Understanding Hypoxemia and Hypocapnia
Hypoxemia is characterized by abnormally low levels of oxygen in the arterial blood, often resulting from respiratory disorders, impaired gas exchange, or high altitudes. Hypocapnia involves reduced carbon dioxide levels in the blood, typically caused by hyperventilation, leading to respiratory alkalosis and altered blood pH. Both conditions disrupt normal respiratory function but affect different gases, requiring distinct diagnostic and treatment approaches tailored to oxygen or carbon dioxide imbalances.
Definitions: Hypoxemia vs Hypocapnia
Hypoxemia is a medical condition characterized by abnormally low levels of oxygen in the arterial blood, generally measured by a partial pressure of oxygen (PaO2) less than 80 mmHg. Hypocapnia refers to decreased carbon dioxide (CO2) levels in the blood, typically defined by a partial pressure of carbon dioxide (PaCO2) below 35 mmHg. These conditions differ fundamentally in their impact on blood gases, with hypoxemia affecting oxygen saturation and hypocapnia primarily influencing respiratory alkalosis.
Causes of Hypoxemia
Hypoxemia, characterized by low arterial oxygen levels, arises primarily from causes such as ventilation-perfusion (V/Q) mismatch, diffusion impairment, hypoventilation, and shunt. Common conditions leading to hypoxemia include chronic obstructive pulmonary disease (COPD), pneumonia, pulmonary embolism, and interstitial lung disease. Unlike hypocapnia, which involves reduced carbon dioxide levels often due to hyperventilation, hypoxemia specifically reflects inadequate oxygenation of blood.
Causes of Hypocapnia
Hypocapnia primarily results from hyperventilation caused by anxiety, pain, or respiratory disorders like asthma and pulmonary embolism. Other causes include metabolic acidosis compensation, fever, and high altitude exposure leading to increased respiratory rate and excessive carbon dioxide elimination. Understanding the pathophysiology of hypocapnia is crucial for differentiating it from hypoxemia, where low blood oxygen levels occur due to impaired gas exchange or ventilation-perfusion mismatch.
Pathophysiological Differences
Hypoxemia refers to abnormally low levels of oxygen in the blood, primarily caused by issues such as ventilation-perfusion mismatch, diffusion impairment, or hypoventilation. Hypocapnia, characterized by decreased carbon dioxide (CO2) levels in the blood, usually results from hyperventilation and affects respiratory drive and cerebral blood flow. The key pathophysiological difference lies in hypoxemia's impact on oxygen delivery to tissues, whereas hypocapnia primarily alters acid-base balance and cerebral vasoconstriction due to reduced CO2.
Clinical Manifestations and Symptoms
Hypoxemia presents primarily with symptoms such as cyanosis, confusion, tachycardia, and shortness of breath due to low arterial oxygen levels. Hypocapnia, characterized by reduced carbon dioxide in the blood, often causes lightheadedness, numbness, muscle cramps, and tetany resulting from respiratory alkalosis. Distinguishing these conditions clinically is critical since hypoxemia reflects inadequate oxygenation, while hypocapnia indicates excessive ventilation leading to altered acid-base balance.
Diagnostic Approaches
Hypoxemia diagnosis primarily involves arterial blood gas (ABG) analysis to measure PaO2 levels, pulse oximetry for peripheral oxygen saturation, and imaging studies like chest X-rays to identify underlying pulmonary causes. Hypocapnia is detected through ABG showing decreased PaCO2 levels, often requiring capnography for continuous monitoring of end-tidal CO2 in respiratory conditions. Both conditions necessitate clinical correlation with patient history and physical examination to distinguish respiratory from metabolic etiologies and guide targeted interventions.
Treatment Strategies
Treatment strategies for hypoxemia prioritize oxygen therapy through nasal cannulas, masks, or mechanical ventilation to restore adequate blood oxygen levels. Hypocapnia management focuses on addressing underlying causes such as hyperventilation, often utilizing controlled breathing techniques or sedation to reduce respiratory rate. Both conditions may require continuous monitoring of arterial blood gases to guide therapy adjustments and ensure effective respiratory support.
Prognosis and Complications
Hypoxemia, characterized by low blood oxygen levels, often leads to severe complications such as organ dysfunction, cognitive impairment, and increased mortality risk if untreated. Hypocapnia, defined by reduced carbon dioxide in the blood, commonly causes respiratory alkalosis, leading to symptoms like dizziness, muscle cramps, and potential seizures but generally has a better prognosis than hypoxemia. Prognosis in hypoxemia depends on severity and underlying cause, while hypocapnia prognosis improves with correction of respiratory imbalance and underlying conditions.
Comparative Summary: Key Takeaways
Hypoxemia refers to low oxygen levels in the blood, while hypocapnia indicates reduced carbon dioxide levels, both affecting respiratory function differently. Hypoxemia often results from impaired oxygen exchange or lung diseases, causing tissue hypoxia and potential organ dysfunction, whereas hypocapnia commonly arises from hyperventilation leading to respiratory alkalosis. Accurate diagnosis relies on arterial blood gas analysis, with treatment strategies targeting the underlying cause to restore normal oxygen and carbon dioxide balance.
Hypoxemia Infographic
 libterm.com
libterm.com