Migraine with aura involves visual or sensory disturbances that typically precede the headache phase, such as flashing lights, zigzag patterns, or numbness. Recognizing these early warning signs helps you manage symptoms and seek timely treatment to reduce the severity of the migraine episode. Explore the rest of this article to learn effective strategies for coping with migraine with aura and improving your quality of life.
Table of Comparison
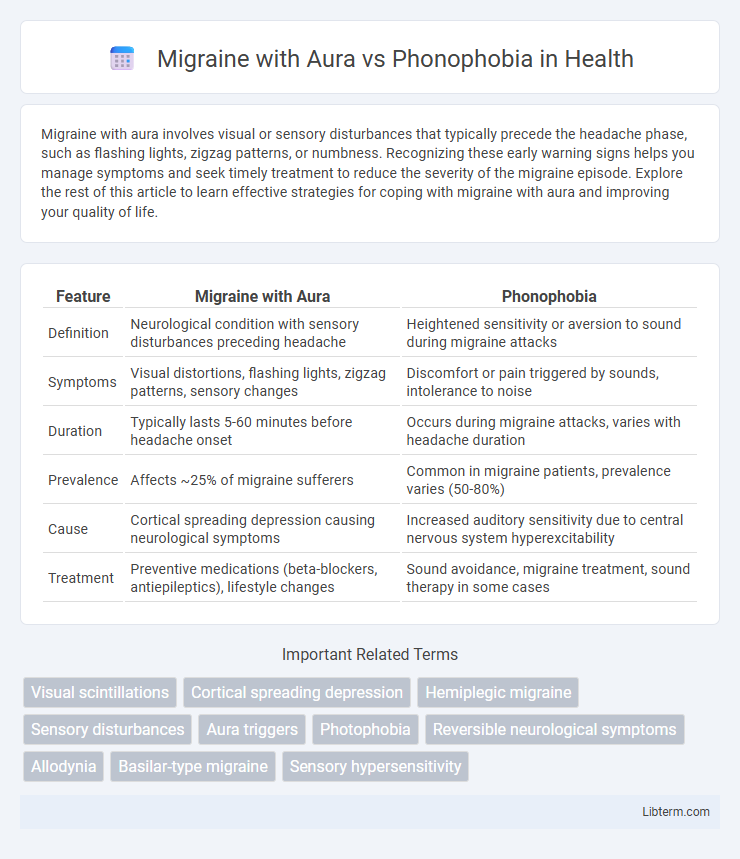
| Feature | Migraine with Aura | Phonophobia |
|---|---|---|
| Definition | Neurological condition with sensory disturbances preceding headache | Heightened sensitivity or aversion to sound during migraine attacks |
| Symptoms | Visual distortions, flashing lights, zigzag patterns, sensory changes | Discomfort or pain triggered by sounds, intolerance to noise |
| Duration | Typically lasts 5-60 minutes before headache onset | Occurs during migraine attacks, varies with headache duration |
| Prevalence | Affects ~25% of migraine sufferers | Common in migraine patients, prevalence varies (50-80%) |
| Cause | Cortical spreading depression causing neurological symptoms | Increased auditory sensitivity due to central nervous system hyperexcitability |
| Treatment | Preventive medications (beta-blockers, antiepileptics), lifestyle changes | Sound avoidance, migraine treatment, sound therapy in some cases |
Understanding Migraine with Aura: Key Features
Migraine with aura is characterized by neurological symptoms such as visual disturbances, sensory changes, and speech difficulties that typically precede the headache phase. Phonophobia, a sensitivity to sound, often accompanies both migraine with aura and migraine without aura but is not exclusive to either type. Key features of migraine with aura include reversible aura symptoms lasting 5 to 60 minutes, unilateral headache following the aura, and significant impairment in daily functioning.
Phonophobia Explained: Sensitivity to Sound
Phonophobia is a heightened sensitivity to sound that often accompanies migraine with aura, causing discomfort or pain in response to everyday noises. This condition is triggered by abnormal neural activity in the brain's auditory processing centers during migraine episodes. Understanding phonophobia in migraine with aura is crucial for effective management and treatment, as it significantly impacts patients' quality of life.
Symptoms Comparison: Migraine with Aura vs Phonophobia
Migraine with aura includes visual disturbances such as flashes of light, blind spots, and sensory changes preceding headache onset, while phonophobia is characterized by an increased sensitivity to sound that often worsens migraine pain. Symptoms of migraine with aura involve neurological signs like tingling or numbness, whereas phonophobia primarily manifests as discomfort or pain triggered by everyday noises. Both conditions contribute to migraine severity but affect different sensory modalities, highlighting the complex symptom spectrum in migraine disorders.
Causes and Triggers: Overlap and Differences
Migraine with aura primarily results from cortical spreading depression, causing neurological symptoms before headache onset, while phonophobia stems from heightened sensory sensitivity linked to central nervous system hyperexcitability. Common triggers for both conditions include stress, hormonal fluctuations, and sensory overload, but migraine with aura is more specifically triggered by visual stimuli and certain foods. Phonophobia uniquely exacerbates due to loud or sudden noises, highlighting a sensory processing difference in migraine pathophysiology.
Neurological Mechanisms Involved
Migraine with aura involves cortical spreading depression (CSD), a wave of neuronal and glial depolarization followed by suppression of brain activity, which triggers the aura symptoms. Phonophobia, common in migraines, results from heightened central nervous system (CNS) sensitivity, particularly increased excitability in the auditory cortex and dysfunctional thalamocortical pathways. Both conditions engage abnormal sensory processing and altered neurotransmitter release, especially involving glutamate and calcitonin gene-related peptide (CGRP), contributing to neuronal hyperexcitability and pain signaling.
Diagnostic Criteria for Each Condition
Migraine with aura is diagnosed based on the presence of reversible neurological symptoms such as visual disturbances, sensory changes, or speech difficulties that precede or accompany headache pain, lasting between 5 to 60 minutes. Phonophobia, characterized by an abnormal sensitivity to sound, is identified through patient history indicating discomfort or pain triggered by normal environmental noise, commonly assessed using audiometric testing. Diagnostic criteria for migraine with aura follow the International Classification of Headache Disorders (ICHD-3), whereas phonophobia is classified as a symptom rather than a standalone diagnosis, requiring careful evaluation of auditory thresholds and patient-reported sensitivity.
Impact on Quality of Life
Migraine with aura significantly impairs quality of life through visual disturbances, sensory sensitivity, and increased disability, often leading to missed workdays and reduced social interaction. Phonophobia, characterized by an intense sensitivity to sound, exacerbates discomfort during migraines, increasing stress and isolation in daily environments. Both conditions contribute to chronic pain management challenges, highlighting the need for targeted therapeutic strategies to improve patient well-being.
Treatment Options: Migraine with Aura
Migraine with Aura treatment options primarily include preventive medications such as beta-blockers, antiepileptic drugs like topiramate, and calcium channel blockers to reduce attack frequency and severity. Acute treatments focus on triptans and nonsteroidal anti-inflammatory drugs (NSAIDs) to alleviate symptoms during an episode, but triptans are contraindicated in patients with aura due to stroke risk. Lifestyle modifications, including stress management, regular sleep patterns, and avoidance of known migraine triggers, complement pharmacologic therapies to improve patient outcomes.
Managing Phonophobia in Migraine Patients
Managing phonophobia in migraine patients requires a multifaceted approach that includes sound therapy, environmental control, and pharmacological interventions. Cognitive-behavioral therapy (CBT) techniques can help patients develop coping strategies to reduce sensitivity to sound triggers, while sound-proofing rooms or using noise-cancelling headphones provides immediate relief during migraine attacks. Medications such as triptans and preventive treatments targeting migraine pathways may also reduce the severity of phonophobia associated with migraine with aura, improving overall quality of life.
Prevention and Lifestyle Strategies
Migraine with aura involves neurological symptoms like visual disturbances preceding headache, while phonophobia refers to heightened sensitivity to sound experienced during migraines. Preventive strategies for migraines with aura emphasize regular sleep patterns, stress management, and avoidance of known triggers such as certain foods or bright lights. Lifestyle modifications including maintaining a quiet environment, using earplugs, and practicing relaxation techniques can effectively reduce phonophobia severity and frequency during migraine episodes.
Migraine with Aura Infographic
 libterm.com
libterm.com