Encephalitis is a serious inflammation of the brain often caused by viral infections or autoimmune reactions. Symptoms can include fever, headache, confusion, seizures, and neurological impairments requiring prompt medical attention. Discover more about encephalitis symptoms, causes, and treatment options in the detailed article ahead.
Table of Comparison
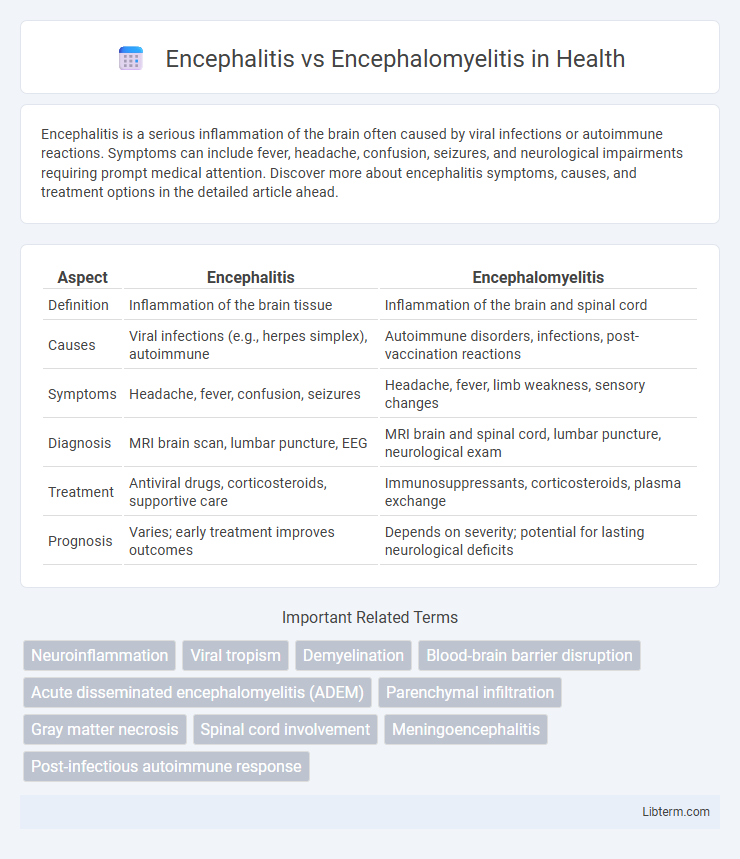
| Aspect | Encephalitis | Encephalomyelitis |
|---|---|---|
| Definition | Inflammation of the brain tissue | Inflammation of the brain and spinal cord |
| Causes | Viral infections (e.g., herpes simplex), autoimmune | Autoimmune disorders, infections, post-vaccination reactions |
| Symptoms | Headache, fever, confusion, seizures | Headache, fever, limb weakness, sensory changes |
| Diagnosis | MRI brain scan, lumbar puncture, EEG | MRI brain and spinal cord, lumbar puncture, neurological exam |
| Treatment | Antiviral drugs, corticosteroids, supportive care | Immunosuppressants, corticosteroids, plasma exchange |
| Prognosis | Varies; early treatment improves outcomes | Depends on severity; potential for lasting neurological deficits |
Introduction to Encephalitis and Encephalomyelitis
Encephalitis is an inflammation of the brain tissue primarily caused by viral infections, leading to symptoms like headache, fever, confusion, and seizures. Encephalomyelitis extends this inflammation to involve both the brain and spinal cord, often resulting from autoimmune reactions or infectious processes that trigger widespread neurological impairment. Distinguishing between encephalitis and encephalomyelitis is critical for accurate diagnosis and targeted treatment strategies in neurology.
Key Differences: Encephalitis vs Encephalomyelitis
Encephalitis primarily refers to the inflammation of the brain tissue, usually caused by viral infections such as herpes simplex virus or arboviruses. Encephalomyelitis involves inflammation of both the brain and spinal cord, often linked to autoimmune disorders or post-infectious reactions like acute disseminated encephalomyelitis (ADEM). Key differences include the anatomical focus--with encephalitis confined to the brain, while encephalomyelitis affects both central nervous system components--and the typical etiologies, where encephalitis is mostly infectious and encephalomyelitis frequently autoimmune or post-infectious.
Causes and Risk Factors
Encephalitis primarily results from viral infections such as herpes simplex virus, West Nile virus, and enteroviruses, with risk factors including weakened immune systems and age extremes. Encephalomyelitis, an inflammation of both the brain and spinal cord, often arises from autoimmune disorders, post-infectious reactions, or vaccinations, with risk factors involving prior infections or immune dysregulation. Both conditions share overlapping causes but differ in their anatomical involvement and specific immune responses.
Common Symptoms and Clinical Presentation
Encephalitis commonly presents with fever, headache, confusion, seizures, and altered mental status, reflecting inflammation primarily of the brain. Encephalomyelitis involves similar neurological symptoms but also includes spinal cord dysfunction such as limb weakness, sensory disturbances, and in severe cases, paralysis, due to combined inflammation of the brain and spinal cord. Both conditions can exhibit symptoms like fever and altered consciousness, but the presence of spinal cord signs helps differentiate encephalomyelitis from encephalitis.
Diagnostic Approaches and Tools
Diagnostic approaches for encephalitis primarily involve magnetic resonance imaging (MRI), cerebrospinal fluid (CSF) analysis via lumbar puncture, and polymerase chain reaction (PCR) testing to identify viral pathogens. Encephalomyelitis diagnosis requires similar tools but places greater emphasis on detecting concurrent spinal cord inflammation through spinal MRI and neurophysiological tests. Both conditions benefit from electroencephalography (EEG) to assess brain function abnormalities and rule out seizures.
Pathophysiology and Affected Areas
Encephalitis primarily involves inflammation of the brain parenchyma, often due to viral infections that trigger immune responses damaging neural tissue. Encephalomyelitis extends inflammation to both the brain and spinal cord, affecting grey and white matter through demyelination and edema, commonly seen in autoimmune or post-infectious conditions. The pathophysiology of encephalomyelitis includes blood-brain barrier disruption and widespread neuroinflammation, whereas encephalitis typically presents with localized neuronal injury confined to cerebral structures.
Treatment Options and Management Strategies
Treatment options for encephalitis primarily include antiviral medications such as acyclovir for herpes simplex virus, alongside supportive care to manage symptoms like seizures and increased intracranial pressure. Encephalomyelitis treatment involves immunosuppressive therapies, including corticosteroids and intravenous immunoglobulins, to reduce inflammation in both the brain and spinal cord. Management strategies emphasize early diagnosis, monitoring neurological status closely, and multidisciplinary rehabilitation to address potential cognitive and motor deficits.
Prognosis and Potential Complications
Encephalitis primarily involves inflammation of the brain tissue, often caused by viral infections, and can lead to long-term neurological deficits such as cognitive impairment or seizures if not treated promptly. Encephalomyelitis, which affects both the brain and spinal cord, tends to have a more severe prognosis due to the combined central nervous system involvement, potentially resulting in paralysis or sensory deficits. Potential complications for both conditions include persistent neurological dysfunction, increased intracranial pressure, and in severe cases, coma or death, highlighting the critical need for early diagnosis and intervention.
Prevention and Risk Reduction
Preventing encephalitis and encephalomyelitis involves reducing exposure to infectious agents such as viruses and bacteria through vaccination, including vaccines for measles, mumps, rubella, and Japanese encephalitis. Employing mosquito control measures and avoiding tick-infested areas also lower the risk since vector-borne infections frequently cause these conditions. Maintaining good personal hygiene, prompt treatment of infections, and managing immune system health further contribute to reducing the likelihood of developing encephalitis or encephalomyelitis.
Frequently Asked Questions
Encephalitis is the inflammation of the brain, primarily caused by viral infections, while encephalomyelitis involves inflammation of both the brain and spinal cord, often related to autoimmune disorders or post-infectious reactions. Common symptoms for both conditions include fever, headache, confusion, and seizures, but encephalomyelitis frequently presents with additional spinal cord-related signs such as limb weakness and sensory disturbances. Diagnosis typically relies on MRI scans, cerebrospinal fluid analysis, and EEG, with treatment focused on antiviral or immunosuppressive therapies tailored to the underlying cause.
Encephalitis Infographic
 libterm.com
libterm.com