Reflux occurs when stomach acid flows back into the esophagus, causing discomfort and potential damage to the lining. Managing reflux effectively involves lifestyle changes and, in some cases, medication to reduce acid production and soothe symptoms. Explore this article to learn how you can identify reflux triggers and find relief for your digestive health.
Table of Comparison
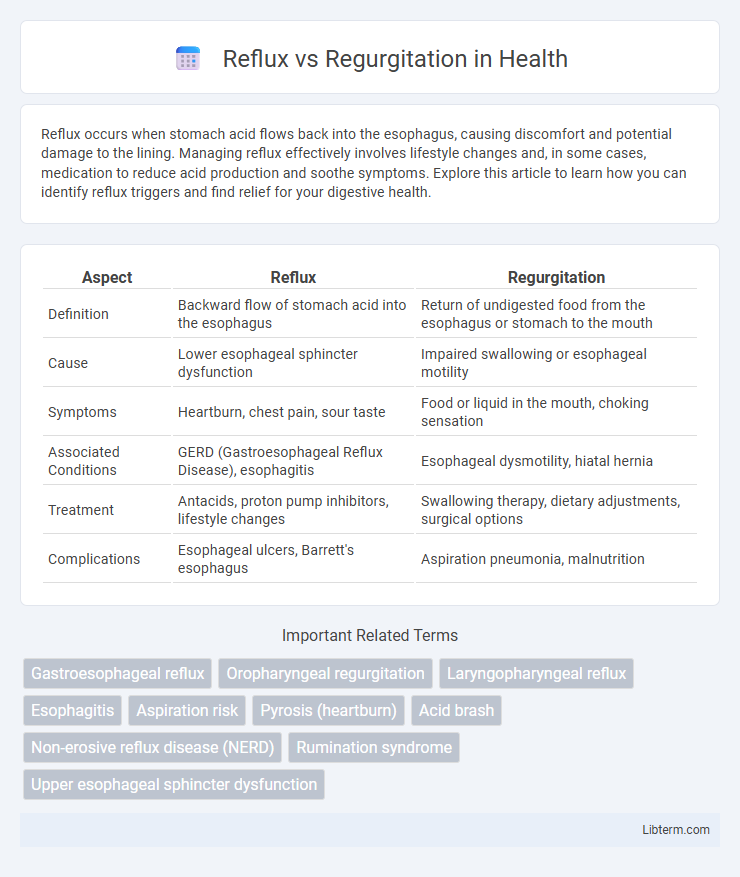
| Aspect | Reflux | Regurgitation |
|---|---|---|
| Definition | Backward flow of stomach acid into the esophagus | Return of undigested food from the esophagus or stomach to the mouth |
| Cause | Lower esophageal sphincter dysfunction | Impaired swallowing or esophageal motility |
| Symptoms | Heartburn, chest pain, sour taste | Food or liquid in the mouth, choking sensation |
| Associated Conditions | GERD (Gastroesophageal Reflux Disease), esophagitis | Esophageal dysmotility, hiatal hernia |
| Treatment | Antacids, proton pump inhibitors, lifestyle changes | Swallowing therapy, dietary adjustments, surgical options |
| Complications | Esophageal ulcers, Barrett's esophagus | Aspiration pneumonia, malnutrition |
Introduction to Reflux and Regurgitation
Reflux refers to the backward flow of stomach contents into the esophagus, often causing symptoms like heartburn and discomfort, and is medically known as gastroesophageal reflux disease (GERD) when chronic. Regurgitation involves the effortless return of undigested food or liquid into the mouth without nausea or retching, commonly observed in infants and related to conditions like esophageal motility disorders. Understanding the distinctions between reflux and regurgitation is essential for accurate diagnosis and appropriate management of these gastrointestinal symptoms.
Defining Reflux: Symptoms and Causes
Reflux occurs when stomach acid flows back into the esophagus, causing symptoms such as heartburn, chest pain, and sour taste in the mouth. Common causes include weak lower esophageal sphincter muscles, obesity, pregnancy, and certain foods or medications that relax the sphincter. Unlike regurgitation, which is the effortless return of undigested food to the mouth, reflux involves acid irritation leading to discomfort and potential esophageal damage.
Understanding Regurgitation: Key Features
Regurgitation involves the effortless, backward flow of undigested food or liquid from the esophagus or stomach into the mouth, often occurring immediately after eating. It differs from reflux by lacking the burning sensation typical of acid exposure, as regurgitated material is usually non-acidic. Key features include a sour or bitter taste, absence of nausea, and the ability to bring up swallowed food without retching or gagging.
Reflux vs Regurgitation: Key Differences
Reflux involves the backflow of stomach acid into the esophagus, causing symptoms such as heartburn and irritation, while regurgitation is the effortless return of undigested food or liquid into the mouth without nausea. Reflux is often associated with gastroesophageal reflux disease (GERD) and may require medical treatment, whereas regurgitation is common in infants and typically resolves without intervention. Diagnosing these conditions relies on symptom patterns, with reflux linked to acid exposure and regurgitation characterized by passive expulsion of contents.
Common Causes of Reflux
Gastroesophageal reflux occurs primarily due to lower esophageal sphincter (LES) dysfunction, where weakened LES muscles allow stomach acid to flow back into the esophagus. Common causes include obesity, hiatal hernia, pregnancy, and certain dietary triggers such as fatty foods, caffeine, and alcohol. Other contributing factors involve delayed gastric emptying and increased intra-abdominal pressure, which exacerbate reflux symptoms.
Common Causes of Regurgitation
Regurgitation commonly results from gastroesophageal reflux disease (GERD), where stomach acid flows back into the esophagus due to a weakened lower esophageal sphincter. Other causes include hiatal hernia, which allows part of the stomach to push into the chest cavity, and esophageal motility disorders that impair normal swallowing and clearance mechanisms. Dietary triggers, obesity, and certain medications can also exacerbate regurgitation symptoms.
Diagnostic Approaches for Reflux and Regurgitation
Diagnostic approaches for reflux primarily include 24-hour pH monitoring, esophageal manometry, and upper endoscopy to evaluate acid exposure, esophageal motility, and mucosal damage. In contrast, regurgitation diagnosis often relies on clinical history and observation, supplemented by barium swallow studies or impedance monitoring to detect non-acidic reflux and evaluate structural abnormalities. Differentiating reflux from regurgitation is critical for targeted treatment, with pH impedance monitoring offering comprehensive analysis of both acid and non-acid reflux episodes.
Treatment Options: Reflux Management
Reflux management primarily involves lifestyle modifications such as dietary changes, weight loss, and avoiding triggers like spicy foods and alcohol. Pharmacological treatments include proton pump inhibitors (PPIs) and H2 receptor antagonists to reduce gastric acid production. In severe cases, surgical interventions like Nissen fundoplication may be recommended to strengthen the lower esophageal sphincter and prevent acid reflux.
Treatment Strategies: Addressing Regurgitation
Treatment strategies addressing regurgitation focus on lifestyle modifications such as dietary changes and elevating the head during sleep to reduce acid exposure. Medications like proton pump inhibitors and H2 receptor antagonists help decrease stomach acid production and alleviate symptoms. In severe cases, surgical interventions such as fundoplication may be recommended to strengthen the lower esophageal sphincter and prevent reflux.
Preventive Tips and Lifestyle Modifications
Reflux prevention involves avoiding trigger foods such as spicy, fatty, and acidic items, maintaining a healthy weight, and eating smaller, frequent meals to reduce stomach pressure. Elevating the head of the bed by 6 to 8 inches and avoiding lying down immediately after eating help minimize acid backflow during sleep. Limiting alcohol intake, quitting smoking, and wearing loose-fitting clothing can further reduce episodes of both acid reflux and regurgitation symptoms.
Reflux Infographic
 libterm.com
libterm.com