Seroma is a medical condition characterized by the accumulation of fluid beneath the skin, often occurring after surgical procedures or trauma. Proper management of seromas is essential to prevent infection and promote healing, involving techniques such as drainage and compression. Discover effective strategies and important information to help you understand and manage seromas in the rest of this article.
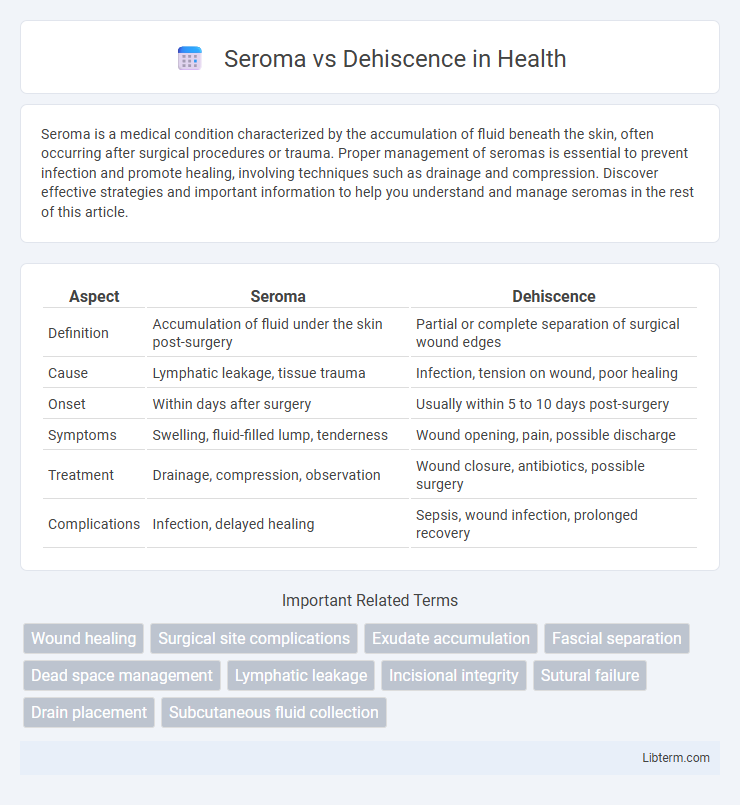
Table of Comparison
| Aspect | Seroma | Dehiscence |
|---|---|---|
| Definition | Accumulation of fluid under the skin post-surgery | Partial or complete separation of surgical wound edges |
| Cause | Lymphatic leakage, tissue trauma | Infection, tension on wound, poor healing |
| Onset | Within days after surgery | Usually within 5 to 10 days post-surgery |
| Symptoms | Swelling, fluid-filled lump, tenderness | Wound opening, pain, possible discharge |
| Treatment | Drainage, compression, observation | Wound closure, antibiotics, possible surgery |
| Complications | Infection, delayed healing | Sepsis, wound infection, prolonged recovery |
Understanding Seroma and Dehiscence
Seroma is a collection of fluid that builds up under the skin after surgery, often appearing as a swollen, soft lump near the incision site, while dehiscence refers to the partial or complete separation of a surgical wound or incision. Both conditions can complicate the healing process, with seroma potentially leading to infection if untreated and dehiscence increasing the risk of wound infection and delayed recovery. Effective management includes proper wound care, monitoring for signs of fluid accumulation or wound opening, and timely medical intervention to prevent complications.
Key Differences Between Seroma and Dehiscence
Seroma refers to the accumulation of fluid at a surgical site, often presenting as a swollen, fluid-filled pocket, whereas dehiscence involves the partial or total reopening of a surgical wound. Seroma primarily results from lymphatic leakage and tissue trauma, while dehiscence is usually caused by mechanical stress, infection, or poor wound healing. Treatment for seroma typically includes drainage and compression, whereas dehiscence often requires wound care, possible surgical intervention, and infection management.
Causes and Risk Factors of Seroma
Seroma formation primarily results from the accumulation of serous fluid in tissue spaces after surgical procedures or trauma, often due to disrupted lymphatic channels and inadequate wound drainage. Risk factors for seroma include extensive tissue dissection, high body mass index (BMI), prolonged operative time, and underlying coagulopathies. Dehiscence, on the other hand, typically arises from poor wound healing caused by infection, increased tension on the wound edges, or systemic conditions like diabetes and malnutrition.
Causes and Risk Factors of Dehiscence
Dehiscence primarily occurs due to poor wound healing caused by factors such as infection, inadequate surgical technique, or excessive tension on wound edges. Risk factors include obesity, diabetes, malnutrition, smoking, and use of corticosteroids, which impair tissue repair and increase susceptibility to wound separation. Unlike seroma, which involves fluid accumulation, dehiscence is characterized by the partial or complete reopening of a surgical incision.
Clinical Signs and Symptoms of Seroma
Seroma presents clinically with localized swelling, palpable fluid-filled sacs beneath the skin, and mild discomfort or tightness at the surgical site. The area may exhibit fluctuation on palpation, with clear or slightly yellow serous fluid upon aspiration. Unlike wound dehiscence, which involves the partial or complete separation of surgical wound edges often accompanied by severe pain, erythema, and possible infection, seromas primarily cause volume-related swelling without wound edge disruption.
Clinical Signs and Symptoms of Dehiscence
Dehiscence is characterized by the partial or complete separation of a surgical incision or wound, often presenting with clinical signs such as increased pain, swelling, and visible gaping of the wound edges. Patients may experience serous or purulent discharge, bleeding, and delayed wound healing, with possible exposure of underlying tissues or organs. Unlike seroma, which primarily involves fluid accumulation without wound separation, dehiscence indicates a significant disruption of wound integrity requiring prompt medical intervention.
Diagnosis: How to Identify Seroma vs Dehiscence
Seroma is identified by the presence of a painless, fluid-filled swelling at a surgical site, typically confirmed through physical examination and ultrasound imaging to detect fluid accumulation. Dehiscence is diagnosed by observing the partial or complete separation of wound edges, often accompanied by redness, discharge, and increased pain, requiring visual inspection and sometimes imaging to assess underlying tissue damage. Accurate differentiation relies on clinical evaluation combined with diagnostic tools like ultrasonography for seroma and wound exploration for dehiscence.
Treatment Approaches for Seroma
Treatment approaches for seroma primarily involve drainage through needle aspiration or placement of a surgical drain to prevent fluid accumulation. Compression dressings and careful monitoring are essential to reduce the risk of infection and promote healing. In refractory cases, sclerotherapy or surgical intervention may be necessary to resolve persistent seromas effectively.
Management and Treatment of Dehiscence
Management of dehiscence involves immediate wound assessment, ensuring proper wound care to prevent infection, and often requires surgical intervention for re-closure. Conservative treatment includes wound cleaning, moist dressings, and monitoring for signs of infection, while severe cases necessitate debridement and secondary closure procedures. Early identification and appropriate treatment reduce complications and promote optimal healing outcomes.
Preventive Strategies for Seroma and Dehiscence
Effective preventive strategies for seroma include meticulous surgical technique to minimize tissue trauma, the use of closed suction drains to evacuate fluid accumulation, and applying compression dressings to reduce dead space. Preventing dehiscence involves ensuring adequate wound closure with tension-free sutures, maintaining aseptic technique to avoid infection, and optimizing patient factors such as nutrition and glycemic control. Both complications benefit from early mobilization and close postoperative monitoring to detect and address issues promptly.
Seroma Infographic
 libterm.com
libterm.com