Acidosis occurs when your body's fluids contain excessive acid, disrupting the natural pH balance and leading to symptoms like fatigue, confusion, and rapid breathing. Identifying the underlying cause, such as respiratory issues or kidney dysfunction, is crucial for effective treatment and preventing complications. Explore the rest of the article to understand acidosis symptoms, causes, and management strategies.
Table of Comparison
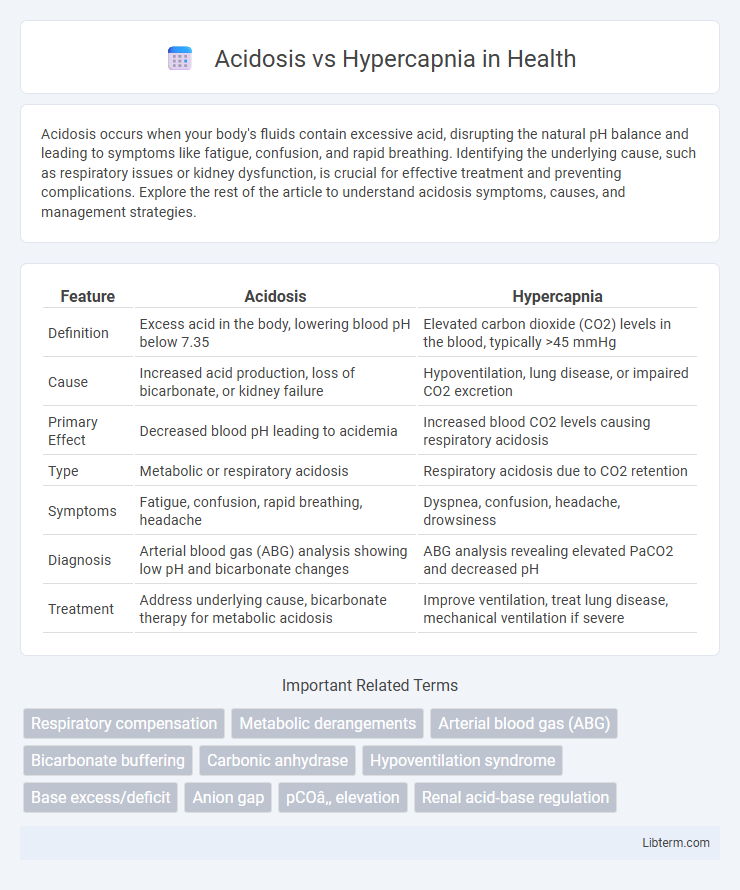
| Feature | Acidosis | Hypercapnia |
|---|---|---|
| Definition | Excess acid in the body, lowering blood pH below 7.35 | Elevated carbon dioxide (CO2) levels in the blood, typically >45 mmHg |
| Cause | Increased acid production, loss of bicarbonate, or kidney failure | Hypoventilation, lung disease, or impaired CO2 excretion |
| Primary Effect | Decreased blood pH leading to acidemia | Increased blood CO2 levels causing respiratory acidosis |
| Type | Metabolic or respiratory acidosis | Respiratory acidosis due to CO2 retention |
| Symptoms | Fatigue, confusion, rapid breathing, headache | Dyspnea, confusion, headache, drowsiness |
| Diagnosis | Arterial blood gas (ABG) analysis showing low pH and bicarbonate changes | ABG analysis revealing elevated PaCO2 and decreased pH |
| Treatment | Address underlying cause, bicarbonate therapy for metabolic acidosis | Improve ventilation, treat lung disease, mechanical ventilation if severe |
Understanding Acidosis: Definition and Types
Acidosis is a physiological condition characterized by an excess of acid in the body fluids, resulting in a blood pH below 7.35. It is classified into two main types: metabolic acidosis, caused by increased acid production or decreased bicarbonate, and respiratory acidosis, resulting from impaired lung function leading to elevated carbon dioxide levels. Understanding these types is crucial for distinguishing acidosis from hypercapnia, where hypercapnia specifically refers to elevated carbon dioxide in the blood, often contributing to respiratory acidosis.
What is Hypercapnia? Causes and Mechanisms
Hypercapnia is the excessive accumulation of carbon dioxide (CO2) in the bloodstream, typically caused by hypoventilation or impaired gas exchange in the lungs. Common causes include chronic obstructive pulmonary disease (COPD), respiratory muscle fatigue, and central nervous system depression, which reduce the body's ability to expel CO2 efficiently. The mechanism involves CO2 retention leading to respiratory acidosis, where increased carbonic acid lowers blood pH and disrupts cellular function.
Key Differences Between Acidosis and Hypercapnia
Acidosis refers to a condition where the blood pH drops below 7.35 due to an excess of hydrogen ions or a loss of bicarbonate, disrupting the body's acid-base balance. Hypercapnia specifically involves elevated levels of carbon dioxide (CO2) in the blood, often resulting from hypoventilation or respiratory failure, and can be a primary cause of respiratory acidosis. The key difference lies in acidosis representing a broader spectrum of acid-base imbalances (metabolic or respiratory), whereas hypercapnia is a specific indicator of respiratory-originating acidosis caused by increased CO2 retention.
Physiological Relationship: How Hypercapnia Causes Acidosis
Hypercapnia, characterized by elevated carbon dioxide (CO2) levels in the blood, directly causes respiratory acidosis by increasing the concentration of carbonic acid through the reaction CO2 + H2O = H2CO3 = H+ + HCO3-. This increase in hydrogen ion (H+) concentration leads to a decrease in blood pH, resulting in acidosis. The body's renal compensation attempts to balance this acid-base disturbance by increasing bicarbonate (HCO3-) reabsorption and hydrogen ion excretion to restore homeostasis.
Clinical Manifestations of Acidosis
Acidosis presents with clinical manifestations such as rapid breathing (tachypnea), confusion, fatigue, and headache due to decreased blood pH affecting enzymatic and cellular function. Severe acidosis may lead to arrhythmias, hypotension, and shock as the cardiovascular system becomes compromised. Identifying these symptoms early ensures prompt management to restore acid-base balance and prevent organ failure.
Signs and Symptoms of Hypercapnia
Hypercapnia, characterized by elevated carbon dioxide levels in the blood, presents with signs such as headache, dizziness, shortness of breath, and confusion. Patients may also experience flushed skin, sweating, increased heart rate, and muscle twitches as hypercapnia progresses. Severe hypercapnia can lead to lethargy, decreased consciousness, and respiratory failure if not promptly addressed.
Diagnostic Approaches: Laboratory and Imaging
Diagnostic approaches for acidosis primarily involve arterial blood gas (ABG) analysis to measure pH, bicarbonate (HCO3-), and partial pressure of carbon dioxide (PaCO2), while hypercapnia is specifically identified by elevated PaCO2 levels. Serum electrolyte panels and lactate levels help determine the underlying cause of metabolic acidosis, whereas chest X-rays and CT scans assist in identifying pulmonary conditions contributing to hypercapnia, such as chronic obstructive pulmonary disease (COPD). Lung function tests, including spirometry, provide additional insight into ventilation abnormalities linked to hypercapnia and respiratory acidosis.
Treatment Strategies: Addressing Acidosis and Hypercapnia
Treatment strategies for acidosis primarily involve correcting the underlying cause and restoring acid-base balance through bicarbonate therapy, renal support, or respiratory interventions. Management of hypercapnia focuses on improving alveolar ventilation using mechanical ventilation, non-invasive positive pressure ventilation, or addressing respiratory muscle fatigue. Both conditions require careful monitoring of arterial blood gases and electrolyte levels to guide therapy and prevent further complications.
Complications and Prognosis for Patients
Acidosis, characterized by a decrease in blood pH, often leads to cellular dysfunction and impaired organ performance, raising the risk of respiratory failure and cardiac arrhythmias. Hypercapnia, marked by elevated arterial carbon dioxide (CO2) levels, can cause respiratory acidosis, resulting in headaches, confusion, and if untreated, progressive respiratory depression. Both conditions require prompt management to prevent severe complications, with prognosis depending on the underlying cause, severity, and timely therapeutic intervention.
Preventive Measures and Patient Management
Preventive measures for acidosis and hypercapnia emphasize regular monitoring of blood gas levels and maintaining proper ventilation to avoid carbon dioxide buildup. Managing patients involves prompt correction of acid-base imbalances through oxygen therapy, mechanical ventilation if necessary, and addressing underlying conditions such as chronic obstructive pulmonary disease (COPD) or renal dysfunction. Nutritional support and careful medication management also play critical roles in stabilizing pH levels and preventing complications.
Acidosis Infographic
 libterm.com
libterm.com