Hypotonic solutions have a lower concentration of solutes compared to the inside of a cell, causing water to move into the cell by osmosis. This influx of water can lead to cell swelling and potentially bursting if the imbalance is severe. Explore the rest of the article to understand how hypotonic environments impact your body and medical treatments.
Table of Comparison
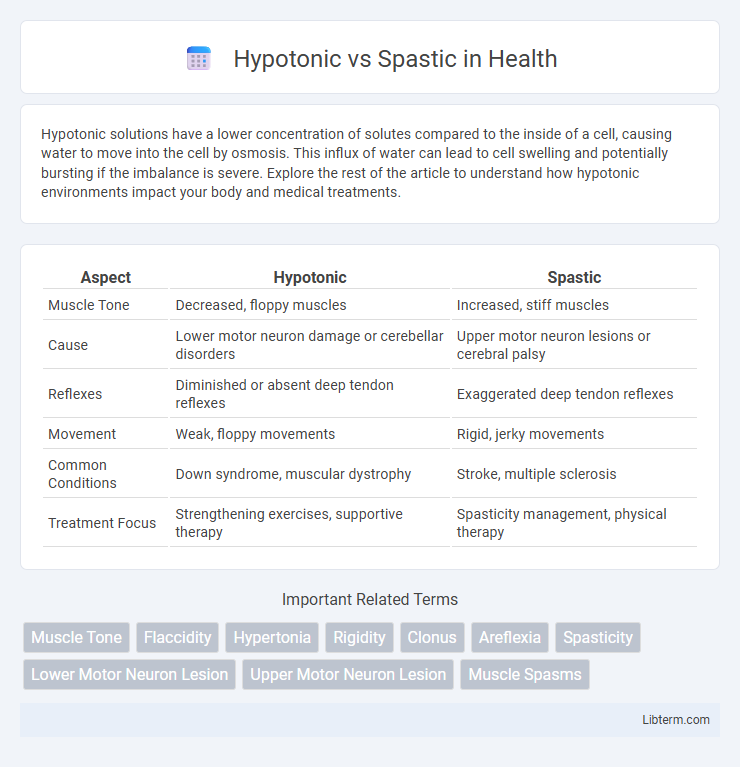
| Aspect | Hypotonic | Spastic |
|---|---|---|
| Muscle Tone | Decreased, floppy muscles | Increased, stiff muscles |
| Cause | Lower motor neuron damage or cerebellar disorders | Upper motor neuron lesions or cerebral palsy |
| Reflexes | Diminished or absent deep tendon reflexes | Exaggerated deep tendon reflexes |
| Movement | Weak, floppy movements | Rigid, jerky movements |
| Common Conditions | Down syndrome, muscular dystrophy | Stroke, multiple sclerosis |
| Treatment Focus | Strengthening exercises, supportive therapy | Spasticity management, physical therapy |
Understanding Muscle Tone: Hypotonic vs Spastic
Muscle tone abnormalities, specifically hypotonic and spastic conditions, are critical in understanding neuromuscular function. Hypotonic muscles exhibit decreased resistance to passive movement, resulting from reduced alpha motor neuron activity or sensory input, commonly seen in conditions like Down syndrome or peripheral neuropathy. Spasticity involves increased muscle tone with hyperactive stretch reflexes, often due to upper motor neuron lesions as found in cerebral palsy or multiple sclerosis, causing stiffness and impaired voluntary movement.
Defining Hypotonicity: Causes and Characteristics
Hypotonicity is characterized by decreased muscle tone, resulting in floppiness and reduced resistance to passive movement. Causes include neurological disorders like cerebral palsy, peripheral nerve damage, and genetic conditions such as Down syndrome or muscular dystrophy. Distinctively, hypotonic muscles lack firmness and struggle with postural control, contrasting with the increased muscle tone and spasticity seen in upper motor neuron lesions.
What is Spasticity? Key Features and Triggers
Spasticity is a motor disorder characterized by an abnormal increase in muscle tone or stiffness, which interferes with movement and is commonly seen in conditions like cerebral palsy, multiple sclerosis, and stroke. Key features include hypertonia, exaggerated tendon reflexes, muscle spasms, and resistance to passive movement. Common triggers for spasticity include sudden movements, infections, stress, cold temperatures, and pain.
Neurological Origins of Hypotonia and Spasticity
Hypotonia results from impaired lower motor neuron or cerebellar dysfunction, leading to decreased muscle tone due to disrupted muscle spindle afferents or synaptic transmission deficits. Spasticity arises from upper motor neuron lesions, particularly in the corticospinal tract, causing hyperexcitability of the stretch reflex and increased muscle tone. Both conditions reflect distinct neuropathological mechanisms, with hypotonia linked to reduced input or output from motor neurons and spasticity associated with disinhibition of spinal reflexes.
Diagnostic Approaches: Hypotonic vs Spastic Presentation
Hypotonic and spastic presentations require distinct diagnostic approaches based on clinical examination and neurophysiological testing. Hypotonia is characterized by diminished muscle tone and reduced resistance to passive stretch, often assessed using the Modified Ashworth Scale and electromyography to differentiate from lower motor neuron lesions. In contrast, spasticity involves velocity-dependent increased muscle tone assessed through clinical scales such as the Tardieu Scale and confirmed via neuroimaging and nerve conduction studies to identify upper motor neuron involvement.
Functional Impacts on Mobility and Movement
Hypotonic muscles exhibit decreased muscle tone, leading to reduced strength and joint stability, which impairs balance and coordinated movement. In contrast, spastic muscles experience increased tone and stiffness, causing involuntary contractions that limit fluidity and range of motion during mobility tasks. These differences significantly affect functional abilities, where hypotonia results in weak and floppy movements, while spasticity frequently causes stiff, jerky, and less controlled motions.
Treatment Options for Hypotonic Conditions
Treatment options for hypotonic conditions primarily include physical and occupational therapy aimed at improving muscle strength and coordination through targeted exercises and stretching routines. Neuromuscular electrical stimulation (NMES) is often utilized to enhance muscle tone and promote neural activation in affected areas. In some cases, pharmacological interventions such as muscle stimulants or medications addressing underlying neurological causes may be prescribed to complement therapy and optimize functional outcomes.
Managing Spasticity: Therapies and Medications
Managing spasticity involves a combination of physical therapies such as stretching, strengthening exercises, and occupational therapy to improve muscle control and reduce stiffness. Pharmacological treatments include baclofen, tizanidine, and botulinum toxin injections, which target muscle overactivity and help alleviate symptoms. Regular assessment by a neurologist or rehabilitation specialist ensures optimal dosage and therapy adjustments tailored to individual patient needs.
Prognosis and Long-Term Outcomes
Hypotonic conditions often present with reduced muscle tone and weakness, leading to delayed motor milestones and potential difficulties in achieving independent movement, with prognosis varying based on underlying etiology. Spasticity, characterized by increased muscle tone and stiffness, frequently results in impaired mobility and joint deformities, requiring ongoing intervention to optimize function and minimize contractures. Long-term outcomes in both conditions depend on early diagnosis, tailored therapy, and multidisciplinary management to maximize physical capabilities and quality of life.
Choosing the Right Support: Hypotonic vs Spastic Care
Choosing the right support for hypotonic versus spastic care hinges on understanding muscle tone differences: hypotonic conditions require interventions that promote muscle activation and increase tone, while spastic care focuses on reducing excessive muscle tightness and preventing contractures. Therapeutic options for hypotonia include active range-of-motion exercises and supportive orthotics designed to enhance stability and strength, whereas spasticity management often involves muscle relaxants, stretching regimens, and customized splints to improve functional mobility. Tailoring care plans with targeted physical therapy and assistive devices ensures optimal outcomes by addressing the distinct neuromuscular challenges in each condition.
Hypotonic Infographic
 libterm.com
libterm.com