Cirrhosis is a chronic liver disease characterized by the gradual replacement of healthy liver tissue with scar tissue, leading to impaired liver function and potential liver failure. Common causes include chronic alcohol abuse, hepatitis infections, and fatty liver disease. Discover how you can recognize symptoms, understand causes, and explore treatment options by reading the rest of this article.
Table of Comparison
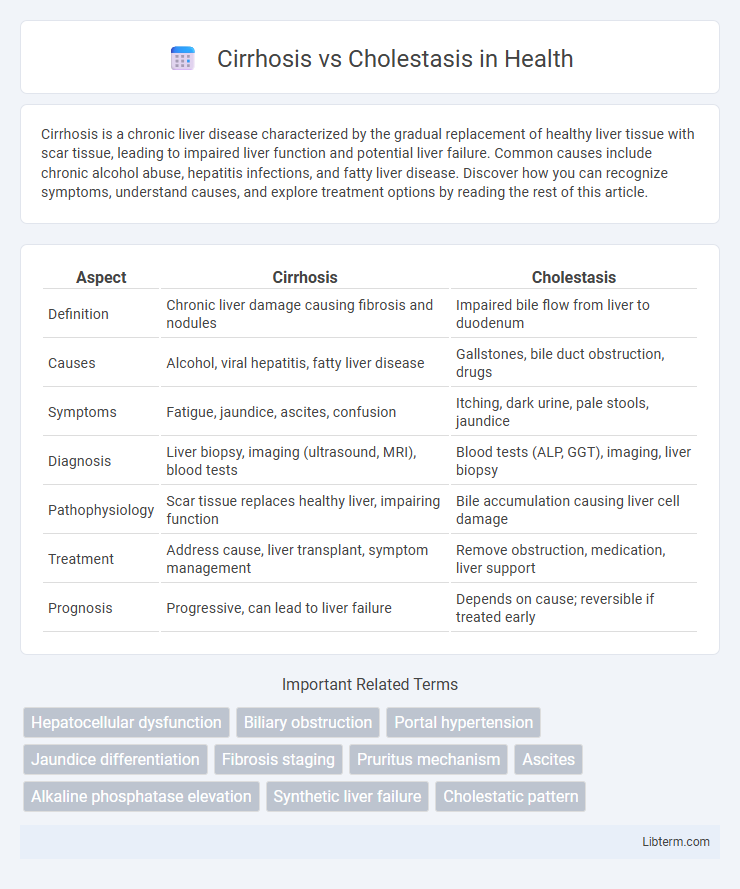
| Aspect | Cirrhosis | Cholestasis |
|---|---|---|
| Definition | Chronic liver damage causing fibrosis and nodules | Impaired bile flow from liver to duodenum |
| Causes | Alcohol, viral hepatitis, fatty liver disease | Gallstones, bile duct obstruction, drugs |
| Symptoms | Fatigue, jaundice, ascites, confusion | Itching, dark urine, pale stools, jaundice |
| Diagnosis | Liver biopsy, imaging (ultrasound, MRI), blood tests | Blood tests (ALP, GGT), imaging, liver biopsy |
| Pathophysiology | Scar tissue replaces healthy liver, impairing function | Bile accumulation causing liver cell damage |
| Treatment | Address cause, liver transplant, symptom management | Remove obstruction, medication, liver support |
| Prognosis | Progressive, can lead to liver failure | Depends on cause; reversible if treated early |
Introduction to Cirrhosis and Cholestasis
Cirrhosis is a progressive liver disease characterized by the replacement of healthy liver tissue with scar tissue, leading to impaired liver function and increased risk of liver failure. Cholestasis involves the reduction or stoppage of bile flow, causing accumulation of bile acids in the liver and subsequent liver damage. Both conditions disrupt normal liver physiology but differ fundamentally in their pathophysiological mechanisms and clinical manifestations.
Understanding Cirrhosis: Definition and Causes
Cirrhosis is a chronic liver disease characterized by irreversible scarring and fibrosis, resulting from sustained liver damage. Common causes include chronic hepatitis B and C infections, excessive alcohol consumption, and non-alcoholic fatty liver disease (NAFLD). This progressive condition impairs liver function by disrupting normal liver architecture and blood flow.
Exploring Cholestasis: Definition and Etiology
Cholestasis refers to the impairment of bile flow from the liver to the duodenum, leading to accumulation of bile acids in the liver and bloodstream. Etiologically, cholestasis can result from intrahepatic causes such as hepatocellular dysfunction, bile duct obstruction due to primary biliary cholangitis, or genetic disorders like Progressive Familial Intrahepatic Cholestasis, as well as extrahepatic causes like gallstones or pancreatic tumors blocking bile ducts. Differentiating cholestasis from cirrhosis is essential as cholestasis primarily involves bile flow disruption, whereas cirrhosis reflects advanced liver fibrosis and architectural distortion.
Key Pathophysiological Differences
Cirrhosis is characterized by progressive liver fibrosis leading to architectural distortion, impaired hepatocyte function, and portal hypertension, whereas cholestasis primarily involves impaired bile flow resulting in bile acid accumulation and hepatocellular injury. In cirrhosis, chronic inflammation and repeated hepatocyte injury cause extensive fibrosis and nodule formation, while cholestasis stems from obstruction or dysfunction of bile ducts causing bile stasis and subsequent bilirubin and lipid retention. The pathophysiological hallmark of cirrhosis is fibrotic scar tissue replacing normal parenchyma, contrasting with cholestasis's disruption of bile secretion and excretion pathways.
Clinical Manifestations: Cirrhosis vs Cholestasis
Cirrhosis clinically presents with symptoms such as jaundice, ascites, spider angiomas, and hepatic encephalopathy due to chronic liver damage and fibrosis. Cholestasis primarily manifests with pruritus, pale stools, dark urine, and jaundice resulting from impaired bile flow and accumulation of bile acids. Both conditions exhibit jaundice, but pruritus is more pronounced in cholestasis, whereas signs of portal hypertension are hallmark features of cirrhosis.
Diagnostic Approaches for Cirrhosis
Diagnostic approaches for cirrhosis primarily involve liver function tests, imaging studies, and histological examination through liver biopsy. Serum biomarkers such as elevated bilirubin, decreased albumin, and prolonged prothrombin time indicate impaired liver function typical of cirrhosis. Ultrasound elastography and transient elastography are non-invasive imaging techniques frequently used to assess liver stiffness, differentiating cirrhosis from other hepatic conditions like cholestasis.
Diagnostic Strategies for Cholestasis
Diagnostic strategies for cholestasis involve a combination of biochemical tests and imaging studies to evaluate bile flow obstruction and liver function. Serum markers such as alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT) are elevated in cholestasis, guiding the need for imaging modalities like ultrasonography, magnetic resonance cholangiopancreatography (MRCP), or endoscopic retrograde cholangiopancreatography (ERCP). Liver biopsy may be utilized in complex cases to differentiate cholestasis from cirrhosis and identify underlying etiologies such as primary biliary cholangitis or primary sclerosing cholangitis.
Treatment Modalities: Cirrhosis vs Cholestasis
Treatment modalities for cirrhosis primarily involve managing complications through medications such as diuretics, beta-blockers, and lactulose, alongside lifestyle changes like alcohol cessation and nutritional support. Cholestasis treatment targets the underlying cause, using ursodeoxycholic acid to improve bile flow, bile acid sequestrants to reduce itching, and procedures like endoscopic retrograde cholangiopancreatography (ERCP) to relieve bile duct obstructions. Liver transplantation may be considered for both conditions when advanced liver damage or liver failure occurs.
Prognosis and Complications
Cirrhosis prognosis varies based on disease stage, with complications like portal hypertension, ascites, and hepatic encephalopathy significantly impacting survival rates and quality of life. Cholestasis prognosis depends on underlying cause and duration, often leading to complications such as bile duct strictures, liver fibrosis, and increased risk of cholangiocarcinoma if untreated. Both conditions require early diagnosis and management to prevent irreversible liver damage and improve clinical outcomes.
Prevention and Patient Management Strategies
Preventing cirrhosis involves controlling risk factors such as chronic alcohol use, viral hepatitis infections (HBV, HCV), and non-alcoholic fatty liver disease through vaccination, antiviral therapy, and lifestyle modifications. Cholestasis prevention centers on managing underlying causes like bile duct obstruction, drug-induced liver injury, and genetic disorders by early diagnosis and tailored medical or surgical interventions. Patient management strategies for cirrhosis emphasize regular monitoring for complications, nutritional support, and potential liver transplantation, while cholestasis management focuses on relieving bile flow obstruction, symptom control, and addressing specific etiologies to prevent progressive liver damage.
Cirrhosis Infographic
 libterm.com
libterm.com