Pancreatitis is a condition characterized by inflammation of the pancreas, causing severe abdominal pain, nausea, and digestive issues. Early diagnosis and appropriate treatment are crucial to prevent complications such as infection, cyst formation, or chronic pancreatitis. Learn more about the symptoms, causes, and management strategies to protect your pancreatic health in the following article.
Table of Comparison
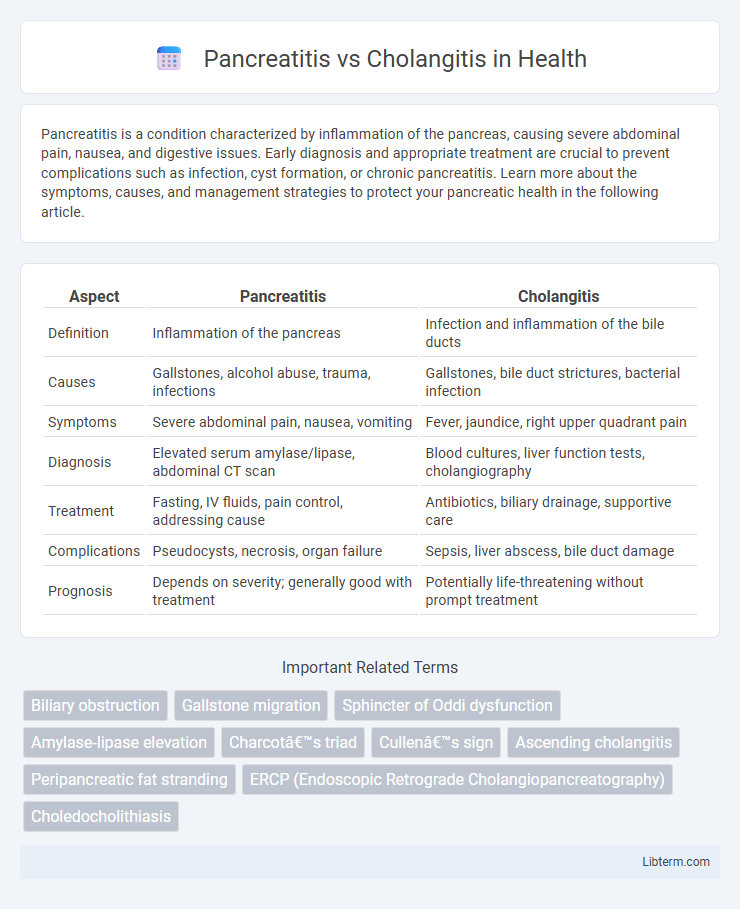
| Aspect | Pancreatitis | Cholangitis |
|---|---|---|
| Definition | Inflammation of the pancreas | Infection and inflammation of the bile ducts |
| Causes | Gallstones, alcohol abuse, trauma, infections | Gallstones, bile duct strictures, bacterial infection |
| Symptoms | Severe abdominal pain, nausea, vomiting | Fever, jaundice, right upper quadrant pain |
| Diagnosis | Elevated serum amylase/lipase, abdominal CT scan | Blood cultures, liver function tests, cholangiography |
| Treatment | Fasting, IV fluids, pain control, addressing cause | Antibiotics, biliary drainage, supportive care |
| Complications | Pseudocysts, necrosis, organ failure | Sepsis, liver abscess, bile duct damage |
| Prognosis | Depends on severity; generally good with treatment | Potentially life-threatening without prompt treatment |
Understanding Pancreatitis and Cholangitis
Pancreatitis is inflammation of the pancreas often caused by gallstones or chronic alcohol use, characterized by severe abdominal pain and elevated pancreatic enzymes. Cholangitis refers to an infection of the bile ducts, typically resulting from bile duct obstruction, with symptoms including jaundice, fever, and right upper quadrant pain. Differentiating these conditions relies on clinical presentation, imaging studies like ultrasound or MRCP, and specific laboratory markers such as elevated liver function tests in cholangitis and increased amylase or lipase levels in pancreatitis.
Causes of Pancreatitis vs Cholangitis
Pancreatitis primarily arises from gallstones obstructing the pancreatic duct or chronic alcohol consumption leading to inflammation of the pancreas. Cholangitis is most commonly caused by bacterial infection following bile duct obstruction, often due to choledocholithiasis or strictures. Both conditions involve biliary tract issues but differ in their pathological origin, with pancreatitis linked to pancreatic enzyme activation and cholangitis associated with biliary infection.
Key Symptoms: How They Differ
Pancreatitis primarily presents with severe upper abdominal pain radiating to the back, accompanied by nausea, vomiting, and elevated pancreatic enzymes like amylase and lipase. In contrast, cholangitis typically manifests with Charcot's triad: fever, right upper quadrant abdominal pain, and jaundice, often linked to biliary obstruction and infection. While pancreatitis pain is more constant and severe, cholangitis symptoms include systemic signs of infection and biliary inflammation, distinguishing the two clinically.
Pathophysiology: What Happens in the Body
Pancreatitis involves inflammation of the pancreas caused by premature activation of digestive enzymes, leading to autodigestion and tissue damage. Cholangitis is characterized by infection and inflammation of the bile ducts, typically resulting from bile duct obstruction and bacterial invasion. Both conditions disrupt normal digestive processes but affect different anatomical structures and trigger distinct inflammatory pathways.
Risk Factors for Each Condition
Pancreatitis risk factors primarily include gallstones, chronic alcohol consumption, hypertriglyceridemia, and certain medications, which contribute to pancreatic inflammation. Cholangitis risk factors encompass biliary obstruction caused by gallstones, bile duct strictures, tumors, or infections, leading to bile duct inflammation and infection. Both conditions share gallstones as a common risk factor, but pancreatitis more often stems from metabolic or toxic causes while cholangitis is largely driven by biliary tract infections and obstructions.
Diagnostic Approaches Compared
Diagnostic approaches for pancreatitis primarily involve serum amylase and lipase tests, with lipase offering higher specificity and sensitivity. In contrast, cholangitis diagnosis relies on liver function tests revealing elevated alkaline phosphatase and bilirubin levels, alongside blood cultures to identify biliary infections. Imaging modalities such as abdominal ultrasound and magnetic resonance cholangiopancreatography (MRCP) are critical in both conditions, but endoscopic retrograde cholangiopancreatography (ERCP) plays a pivotal role in confirming and treating cholangitis by visualizing and relieving biliary obstructions.
Treatment Options: Pancreatitis vs Cholangitis
Treatment options for pancreatitis primarily involve fasting, intravenous fluids, pain management, and addressing underlying causes like gallstones or alcohol use, with severe cases requiring endoscopic or surgical intervention. Cholangitis treatment centers on prompt antibiotic therapy to combat infection combined with biliary drainage procedures such as endoscopic retrograde cholangiopancreatography (ERCP) to relieve obstruction. Both conditions necessitate tailored approaches based on severity and etiology, emphasizing timely intervention to prevent complications.
Potential Complications and Prognosis
Pancreatitis can lead to complications such as necrosis, pseudocysts, and systemic inflammatory response syndrome (SIRS), often resulting in prolonged hospitalization and varying degrees of organ failure, with prognosis depending on severity and timely intervention. Cholangitis commonly causes complications like sepsis, biliary abscesses, and liver failure, where early antibiotic treatment and biliary drainage improve outcomes but delays significantly worsen prognosis. Both conditions require immediate medical attention to minimize risks, yet pancreatitis has a more variable recovery trajectory compared to the typically acute and potentially life-threatening nature of cholangitis complications.
Prevention Strategies for Both Diseases
Effective prevention strategies for pancreatitis involve avoiding excessive alcohol consumption, maintaining a healthy diet low in fat, and managing gallstone risk through regular medical checkups. For cholangitis, prevention centers on early treatment of biliary obstructions, including gallstones and strictures, along with timely antibiotic therapy to reduce infection risk. Both diseases benefit from prompt intervention and lifestyle modifications aimed at reducing inflammation and biliary tract complications.
When to Seek Immediate Medical Attention
Severe abdominal pain, persistent vomiting, and high fever indicate potential pancreatitis or cholangitis requiring immediate medical attention to prevent complications like organ failure or sepsis. Jaundice, altered mental status, or rapid heart rate in cholangitis patients signal acute cholangitis emergencies needing urgent intervention. Early diagnosis through imaging and blood tests is critical to initiate treatments such as antibiotics for cholangitis or supportive care for pancreatitis, improving patient outcomes.
Pancreatitis Infographic
 libterm.com
libterm.com