Pneumonia is a serious respiratory infection that inflames the air sacs in one or both lungs, which may fill with fluid or pus, causing symptoms like coughing, fever, chills, and difficulty breathing. Prompt diagnosis and treatment with antibiotics or antiviral medications are crucial to prevent complications and ensure a full recovery. Explore this article to learn more about pneumonia's causes, symptoms, treatment options, and prevention tips to protect your health.
Table of Comparison
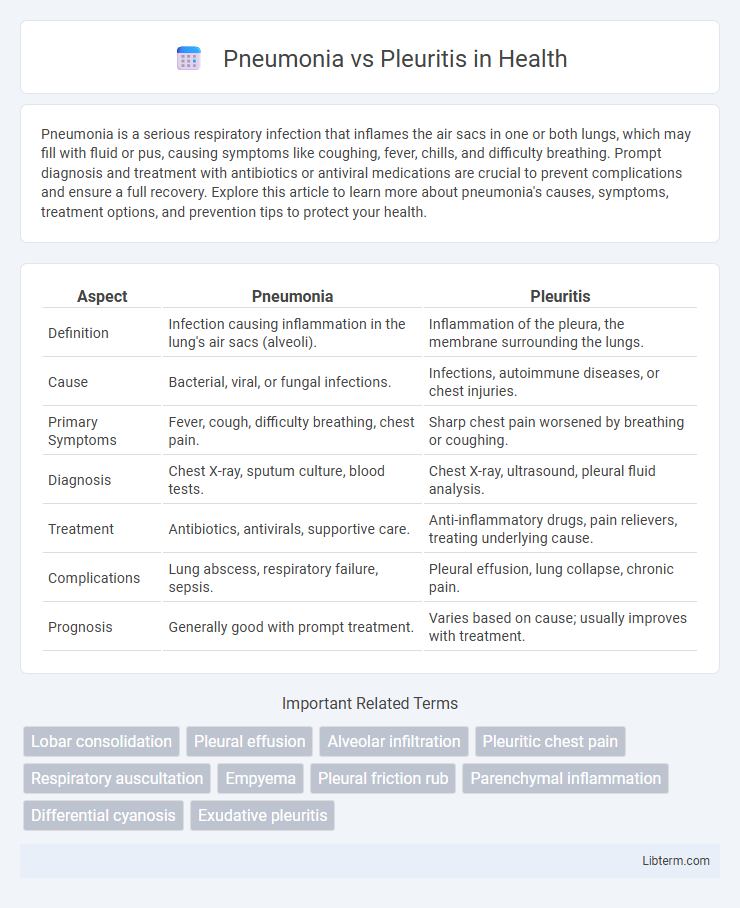
| Aspect | Pneumonia | Pleuritis |
|---|---|---|
| Definition | Infection causing inflammation in the lung's air sacs (alveoli). | Inflammation of the pleura, the membrane surrounding the lungs. |
| Cause | Bacterial, viral, or fungal infections. | Infections, autoimmune diseases, or chest injuries. |
| Primary Symptoms | Fever, cough, difficulty breathing, chest pain. | Sharp chest pain worsened by breathing or coughing. |
| Diagnosis | Chest X-ray, sputum culture, blood tests. | Chest X-ray, ultrasound, pleural fluid analysis. |
| Treatment | Antibiotics, antivirals, supportive care. | Anti-inflammatory drugs, pain relievers, treating underlying cause. |
| Complications | Lung abscess, respiratory failure, sepsis. | Pleural effusion, lung collapse, chronic pain. |
| Prognosis | Generally good with prompt treatment. | Varies based on cause; usually improves with treatment. |
Understanding Pneumonia and Pleuritis: Key Differences
Pneumonia is an infection causing inflammation in the lung's air sacs, often triggered by bacteria, viruses, or fungi, leading to symptoms like cough, fever, and difficulty breathing. Pleuritis, also known as pleurisy, involves inflammation of the pleura, the membrane surrounding the lungs, causing sharp chest pain that worsens with breathing or coughing. Understanding these conditions requires noting pneumonia primarily affects lung tissue, while pleuritis impacts the pleural lining, with distinct causes, symptoms, and diagnostic approaches.
Causes of Pneumonia vs Pleuritis
Pneumonia is primarily caused by bacterial, viral, or fungal infections that lead to inflammation of the lung tissue, with common pathogens including Streptococcus pneumoniae and influenza viruses. Pleuritis, also known as pleurisy, results from inflammation of the pleura, often triggered by viral infections, pulmonary embolism, or autoimmune diseases like lupus. While pneumonia involves infection within the lung parenchyma, pleuritis stems from irritation or inflammation of the pleural layers surrounding the lungs.
Common Symptoms: Pneumonia vs Pleuritis
Pneumonia commonly presents with cough, fever, chills, and shortness of breath, accompanied by chest pain that worsens with deep breathing or coughing. Pleuritis, also known as pleurisy, typically causes sharp, stabbing chest pain that intensifies during inhalation, alongside symptoms such as dry cough and fever. Both conditions can cause pleuritic chest pain and respiratory discomfort, but pneumonia often includes systemic signs of infection, while pleuritis primarily involves localized chest pain.
Risk Factors and Populations at Risk
Pneumonia primarily affects older adults, infants, and individuals with weakened immune systems, with risk factors including smoking, chronic lung disease, and recent respiratory infections. Pleuritis, often associated with autoimmune disorders, viral infections, or pulmonary embolism, poses a higher risk to patients with rheumatoid arthritis, lupus, and other systemic inflammatory conditions. Both conditions require prompt medical evaluation, especially in populations with underlying health vulnerabilities and compromised respiratory defenses.
Diagnostic Approaches for Pneumonia and Pleuritis
Diagnostic approaches for pneumonia primarily involve chest X-rays to identify lung infiltrates, sputum cultures to detect causative pathogens, and blood tests to assess inflammatory markers such as elevated white blood cell count and C-reactive protein. Pleuritis diagnosis relies on clinical examination revealing pleuritic chest pain and pleural friction rub, complemented by imaging studies like chest ultrasound and pleural fluid analysis obtained via thoracentesis to distinguish infectious from non-infectious causes. Both conditions may require additional tests such as CT scans for detailed visualization and to rule out complications or alternative diagnoses.
Treatment Options: Pneumonia vs Pleuritis
Treatment options for pneumonia primarily involve antibiotics targeting the causative bacterial pathogens, with supportive care such as oxygen therapy and fluids to manage symptoms. Pleuritis treatment focuses on addressing the underlying cause, often using nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief and corticosteroids in severe cases. Both conditions may require hospitalization if complications arise, but pneumonia treatment emphasizes infection control while pleuritis centers on inflammation reduction.
Complications Associated with Each Condition
Pneumonia often leads to complications such as lung abscesses, respiratory failure, sepsis, and pleural effusion, which can worsen patient outcomes and require intensive medical management. Pleuritis, or pleurisy, primarily results in complications like pleural effusion, pneumothorax, and in some cases, chronic pleural thickening, potentially causing persistent chest pain and impaired lung function. Early diagnosis and targeted treatment are essential to prevent the progression of these complications and reduce morbidity associated with both conditions.
Prevention Strategies for Pneumonia and Pleuritis
Pneumonia prevention strategies include vaccination with pneumococcal and influenza vaccines, maintaining good hand hygiene, and avoiding smoking to reduce lung vulnerability. Pleuritis prevention focuses on controlling underlying respiratory infections and preventing complications from viral or bacterial illnesses through timely treatment. Both conditions benefit from maintaining a healthy immune system and prompt medical attention to respiratory symptoms to reduce the risk of severe inflammation.
Prognosis and Recovery Time
Pneumonia prognosis depends on factors such as age, comorbidities, and causative pathogens, with recovery typically ranging from 1 to 3 weeks following appropriate antibiotic or antiviral treatment. Pleuritis prognosis is generally favorable when the underlying cause is treated, and symptoms often resolve within a few days to weeks, although chronic or recurrent pleuritis may prolong recovery. Both conditions require timely medical intervention to prevent complications, but pneumonia generally poses a higher risk of severe outcomes and longer rehabilitation periods.
When to Seek Medical Help
Seek medical help immediately if you experience high fever, severe chest pain, difficulty breathing, or persistent cough, as these symptoms may indicate pneumonia or pleuritis complications. Pneumonia often requires prompt antibiotic treatment to prevent lung damage, while pleuritis may need anti-inflammatory medication and diagnostic imaging to assess pleural involvement. Early medical intervention is crucial to avoid severe respiratory issues or pleural effusion associated with both conditions.
Pneumonia Infographic
 libterm.com
libterm.com