Diabetes mellitus is a chronic condition characterized by high blood sugar levels due to the body's inability to produce or effectively use insulin. Proper management includes lifestyle changes, medication, and regular monitoring to prevent complications such as heart disease and nerve damage. Explore the article to understand how you can better manage diabetes mellitus and improve your health outcomes.
Table of Comparison
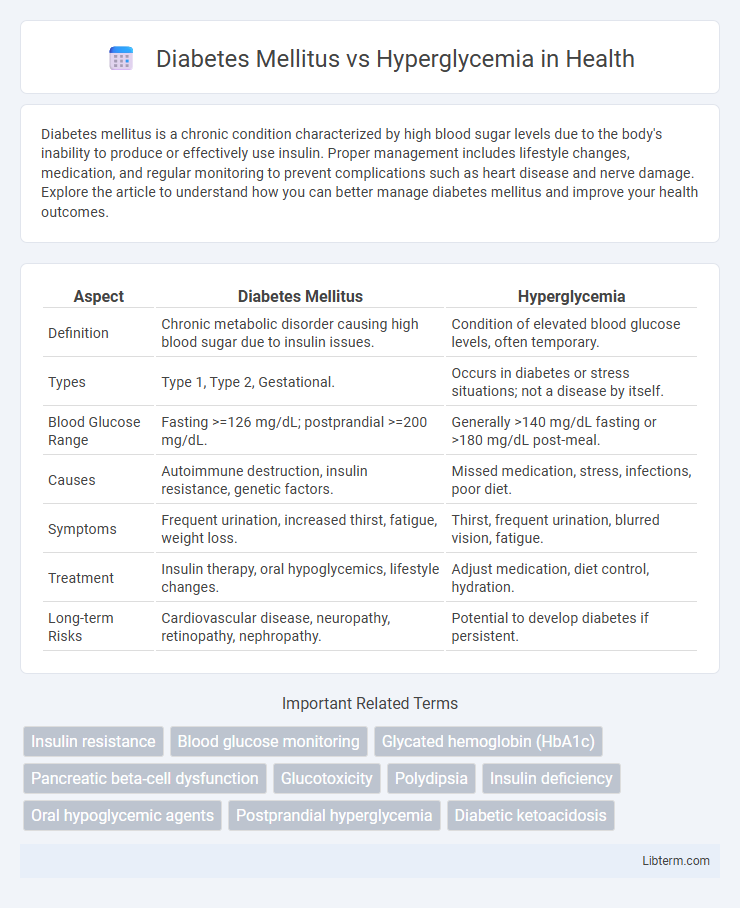
| Aspect | Diabetes Mellitus | Hyperglycemia |
|---|---|---|
| Definition | Chronic metabolic disorder causing high blood sugar due to insulin issues. | Condition of elevated blood glucose levels, often temporary. |
| Types | Type 1, Type 2, Gestational. | Occurs in diabetes or stress situations; not a disease by itself. |
| Blood Glucose Range | Fasting >=126 mg/dL; postprandial >=200 mg/dL. | Generally >140 mg/dL fasting or >180 mg/dL post-meal. |
| Causes | Autoimmune destruction, insulin resistance, genetic factors. | Missed medication, stress, infections, poor diet. |
| Symptoms | Frequent urination, increased thirst, fatigue, weight loss. | Thirst, frequent urination, blurred vision, fatigue. |
| Treatment | Insulin therapy, oral hypoglycemics, lifestyle changes. | Adjust medication, diet control, hydration. |
| Long-term Risks | Cardiovascular disease, neuropathy, retinopathy, nephropathy. | Potential to develop diabetes if persistent. |
Understanding Diabetes Mellitus: Definition and Types
Diabetes Mellitus is a chronic metabolic disorder characterized by high blood glucose levels due to impaired insulin production or action, primarily classified into Type 1, Type 2, and gestational diabetes. Type 1 diabetes results from autoimmune destruction of pancreatic beta cells, leading to absolute insulin deficiency, while Type 2 diabetes involves insulin resistance combined with relative insulin deficiency. Gestational diabetes occurs during pregnancy and poses risks for both mother and child, highlighting the importance of early diagnosis and management.
What is Hyperglycemia? Causes and Risk Factors
Hyperglycemia refers to elevated blood glucose levels, typically above 130 mg/dL fasting or 180 mg/dL post-meal, and is a common symptom of diabetes mellitus. Causes of hyperglycemia include insufficient insulin production, insulin resistance, stress, illness, and certain medications. Risk factors encompass obesity, sedentary lifestyle, family history of diabetes, and poor dietary habits high in refined sugars and carbohydrates.
Key Differences Between Diabetes Mellitus and Hyperglycemia
Diabetes mellitus is a chronic metabolic disorder characterized by persistent high blood glucose levels due to insulin deficiency or resistance, whereas hyperglycemia refers specifically to an acute or temporary elevation of blood glucose above normal levels. Diabetes mellitus encompasses both type 1 and type 2 conditions with systemic effects, while hyperglycemia can occur as a symptom of diabetes or other medical situations without constituting a standalone disease. Diagnosis of diabetes involves criteria like fasting plasma glucose >=126 mg/dL or HbA1c >=6.5%, whereas hyperglycemia is identified by transient glucose spikes often exceeding 180 mg/dL during postprandial monitoring.
Common Symptoms: Recognizing the Signs
Diabetes Mellitus and hyperglycemia share common symptoms such as frequent urination, increased thirst, and unexplained weight loss, indicating elevated blood glucose levels. Both conditions often cause fatigue, blurred vision, and slow wound healing due to impaired glucose metabolism and vascular complications. Early recognition of these signs is crucial for timely diagnosis and management to prevent severe complications like neuropathy and retinopathy.
Underlying Mechanisms: Pathophysiology Compared
Diabetes Mellitus is a chronic metabolic disorder characterized by impaired insulin production or action, leading to persistent hyperglycemia, whereas hyperglycemia refers specifically to elevated blood glucose levels regardless of underlying cause. The pathophysiology of Diabetes Mellitus involves autoimmune destruction of pancreatic beta cells in Type 1 or insulin resistance in peripheral tissues in Type 2, resulting in systemic glucose dysregulation. Hyperglycemia can arise from multiple mechanisms including stress responses, endocrine disorders, or medication effects, and does not necessarily indicate Diabetes Mellitus unless sustained by the core insulin disturbances.
Diagnosis: Tests and Criteria for Each Condition
Diabetes Mellitus diagnosis relies on fasting plasma glucose >=126 mg/dL, 2-hour plasma glucose >=200 mg/dL during an oral glucose tolerance test, or HbA1c >=6.5%. Hyperglycemia is identified by elevated blood glucose levels above normal thresholds but below diabetes diagnostic criteria, often detected through random plasma glucose tests exceeding 140 mg/dL. Continuous glucose monitoring and postprandial glucose measurements help distinguish transient hyperglycemia from chronic diabetes mellitus.
Management Strategies: Diabetes Mellitus vs Hyperglycemia
Management strategies for Diabetes Mellitus involve comprehensive approaches including lifestyle modifications, blood glucose monitoring, and pharmacotherapy such as insulin or oral hypoglycemic agents to maintain long-term glycemic control. In contrast, hyperglycemia treatment focuses on acute correction through hydration, electrolyte balance, and short-term insulin administration to prevent complications like diabetic ketoacidosis. Both conditions require individualized care plans emphasizing regular monitoring and addressing underlying causes to optimize patient outcomes.
Complications and Long-Term Risks
Diabetes mellitus, characterized by chronic hyperglycemia, significantly increases the risk of complications such as neuropathy, retinopathy, nephropathy, and cardiovascular disease due to prolonged high blood glucose levels. Hyperglycemia, including transient or episodic elevations in blood sugar, can exacerbate oxidative stress and inflammation, accelerating vascular damage and increasing the likelihood of long-term organ dysfunction. Persistent hyperglycemia in diabetes leads to microvascular and macrovascular complications, substantially impacting morbidity and mortality rates worldwide.
Prevention Tips and Lifestyle Modifications
Effective prevention of Diabetes Mellitus involves maintaining a balanced diet rich in whole grains, vegetables, and lean proteins while limiting sugar and refined carbohydrates to regulate blood glucose levels. Regular physical activity, such as 150 minutes of moderate exercise per week, enhances insulin sensitivity and helps prevent hyperglycemia. Monitoring body weight, avoiding tobacco use, and managing stress through mindfulness or therapy contribute significantly to reducing the risk of both Diabetes Mellitus and hyperglycemia episodes.
When to Seek Medical Attention and Treatment Options
Seek medical attention for Diabetes Mellitus when experiencing persistent high blood sugar levels, frequent urination, excessive thirst, unexplained weight loss, or symptoms of diabetic ketoacidosis such as nausea and confusion. Hyperglycemia requires prompt evaluation if blood glucose rises above 180 mg/dL consistently, especially with symptoms like fatigue, blurred vision, or slow wound healing. Treatment options for Diabetes Mellitus include lifestyle changes, oral hypoglycemic agents, and insulin therapy, while hyperglycemia management focuses on adjusting medications, dietary modifications, and monitoring blood glucose to prevent complications.
Diabetes Mellitus Infographic
 libterm.com
libterm.com