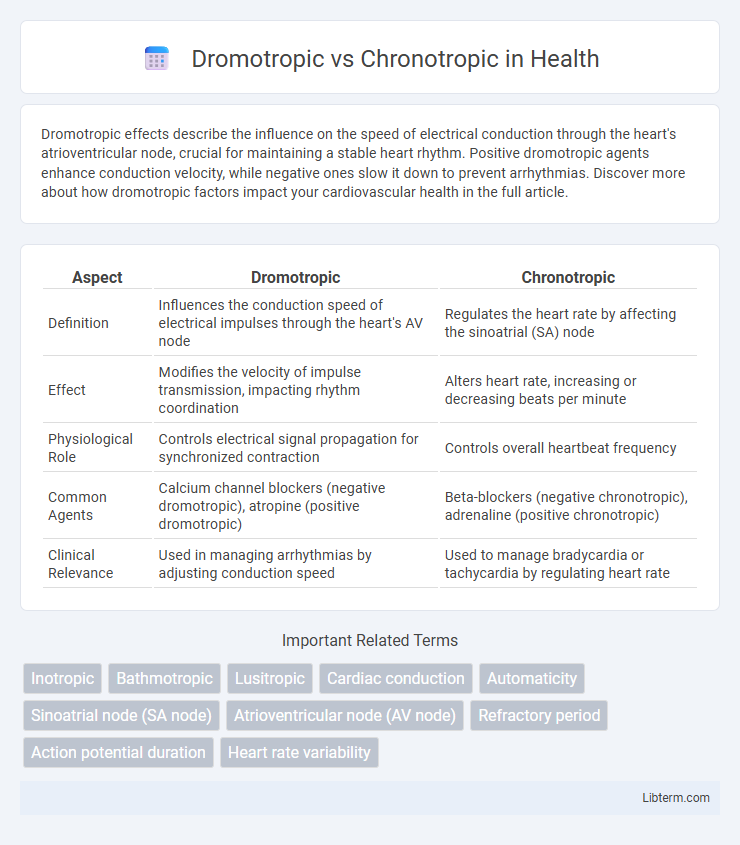
Dromotropic effects describe the influence on the speed of electrical conduction through the heart's atrioventricular node, crucial for maintaining a stable heart rhythm. Positive dromotropic agents enhance conduction velocity, while negative ones slow it down to prevent arrhythmias. Discover more about how dromotropic factors impact your cardiovascular health in the full article.
Table of Comparison
| Aspect | Dromotropic | Chronotropic |
|---|---|---|
| Definition | Influences the conduction speed of electrical impulses through the heart's AV node | Regulates the heart rate by affecting the sinoatrial (SA) node |
| Effect | Modifies the velocity of impulse transmission, impacting rhythm coordination | Alters heart rate, increasing or decreasing beats per minute |
| Physiological Role | Controls electrical signal propagation for synchronized contraction | Controls overall heartbeat frequency |
| Common Agents | Calcium channel blockers (negative dromotropic), atropine (positive dromotropic) | Beta-blockers (negative chronotropic), adrenaline (positive chronotropic) |
| Clinical Relevance | Used in managing arrhythmias by adjusting conduction speed | Used to manage bradycardia or tachycardia by regulating heart rate |
Introduction to Cardiac Conduction System
The cardiac conduction system regulates heart rhythm through specialized tissues including the sinoatrial (SA) node, atrioventricular (AV) node, bundle of His, and Purkinje fibers. Chronotropic effects influence heart rate by modifying the SA node's firing rate, while dromotropic effects alter the speed of electrical impulse conduction primarily through the AV node. Understanding these mechanisms is essential for assessing cardiac function and managing arrhythmias.
Defining Dromotropic Effects
Dromotropic effects refer to the influence on the conduction velocity of electrical impulses through the heart's atrioventricular (AV) node, directly impacting the speed at which signals travel between the atria and ventricles. Positive dromotropic agents, such as catecholamines, increase conduction velocity, enhancing the heart's ability to respond to increased demand, while negative dromotropic agents, like beta-blockers, slow AV node conduction. Understanding dromotropic effects is crucial for managing arrhythmias and optimizing cardiac output in clinical cardiology.
Understanding Chronotropic Effects
Chronotropic effects refer to the influence on heart rate by altering the timing of cardiac pacemaker activity, primarily impacting the sinoatrial node. Positive chronotropic agents increase heart rate by accelerating the rate of depolarization, while negative chronotropic agents slow the heart rate by decreasing pacemaker activity. Understanding these effects is crucial for the management of arrhythmias and optimizing cardiac output in various clinical settings.
Key Differences: Dromotropic vs. Chronotropic
Dromotropic effects refer to the influence on the conduction velocity of electrical impulses through the heart's atrioventricular node, while chronotropic effects pertain to the modulation of heart rate by altering the pacemaker activity of the sinoatrial node. Positive dromotropic agents increase conduction speed, improving synchronization of cardiac contractions, whereas positive chronotropic agents elevate heart rate, enhancing cardiac output during stress or exercise. Understanding these distinctions is critical for targeted cardiovascular therapies, especially in managing arrhythmias and heart failure.
Physiological Mechanisms Behind Each Effect
Dromotropic effects involve the modulation of electrical conduction velocity through the atrioventricular (AV) node primarily influenced by the autonomic nervous system and ion channel activity, particularly affecting calcium and potassium channels. Chronotropic effects regulate heart rate by altering the rate of spontaneous depolarization in the sinoatrial (SA) node through changes in pacemaker current (If) and sympathetic or parasympathetic stimulation. Both effects are crucial in cardiac electrophysiology, with dromotropic mechanisms impacting impulse propagation speed and chronotropic mechanisms controlling heartbeat frequency.
Clinical Significance and Examples
Dromotropic and chronotropic effects directly influence cardiac function by altering conduction velocity and heart rate, respectively, critical in managing arrhythmias and heart failure. Clinically, positive dromotropic agents like isoproterenol enhance atrioventricular node conduction, beneficial in heart block scenarios, while negative dromotropes such as calcium channel blockers slow conduction to prevent tachyarrhythmias. Chronotropic modulation, seen with beta-blockers reducing heart rate or atropine increasing it, helps optimize cardiac output and manage bradycardia or tachycardia conditions.
Pharmacological Agents Impacting Dromotropic Activity
Pharmacological agents impacting dromotropic activity primarily influence the conduction velocity through the atrioventricular (AV) node, with negative dromotropic drugs such as beta-blockers (e.g., propranolol) and calcium channel blockers (e.g., verapamil) slowing AV nodal conduction to treat arrhythmias. Positive dromotropic agents, including catecholamines like dopamine and dobutamine, enhance AV nodal conduction by increasing intracellular calcium, facilitating faster impulse propagation. Understanding the specific dromotropic effects of these pharmacological agents is crucial for managing cardiac rhythm disorders and optimizing therapeutic interventions.
Drugs and Substances Affecting Chronotropic Responses
Drugs affecting chronotropic responses primarily influence heart rate by targeting the sinoatrial node, with beta-adrenergic agonists like isoproterenol increasing heart rate and beta-blockers such as propranolol decreasing it. Calcium channel blockers, including verapamil and diltiazem, also exhibit negative chronotropic effects by reducing nodal conduction velocity and slowing heart rate. Substances like atropine act as anticholinergics to increase heart rate by inhibiting parasympathetic influence on the heart.
Diagnostic and Therapeutic Implications
Dromotropic effects influence the conduction velocity through the atrioventricular node, critically assessed via electrocardiograms to diagnose arrhythmias and guide therapeutic pacing strategies. Chronotropic effects alter heart rate by modulating sinoatrial node activity, serving as key indicators in evaluating sinus node dysfunction and tailoring beta-blocker or pacemaker treatments. Understanding these distinctions optimizes clinical management of cardiac conduction disorders and informs precise pharmacological interventions.
Summary: Integrating Dromotropic and Chronotropic Concepts
Dromotropic and chronotropic effects are critical in regulating cardiac function, where dromotropic refers to the conduction velocity of electrical impulses through the heart's AV node, and chronotropic pertains to the heart rate modulation. Integrating these concepts is essential for understanding how drugs like beta-blockers or calcium channel blockers influence both the speed of electrical conduction and heart rate to optimize cardiac output and treat arrhythmias. Precise modulation of dromotropic and chronotropic parameters enables targeted management of conditions such as atrial fibrillation and heart failure by balancing conduction speed and pacing rate.
Dromotropic Infographic
 libterm.com
libterm.com