Sleep paralysis occurs when your mind wakes up before your body, leaving you temporarily unable to move or speak while falling asleep or waking up. This phenomenon can be accompanied by vivid hallucinations and a sense of pressure on the chest, often causing fear and confusion. Discover effective strategies to manage sleep paralysis and regain control by reading the rest of this article.
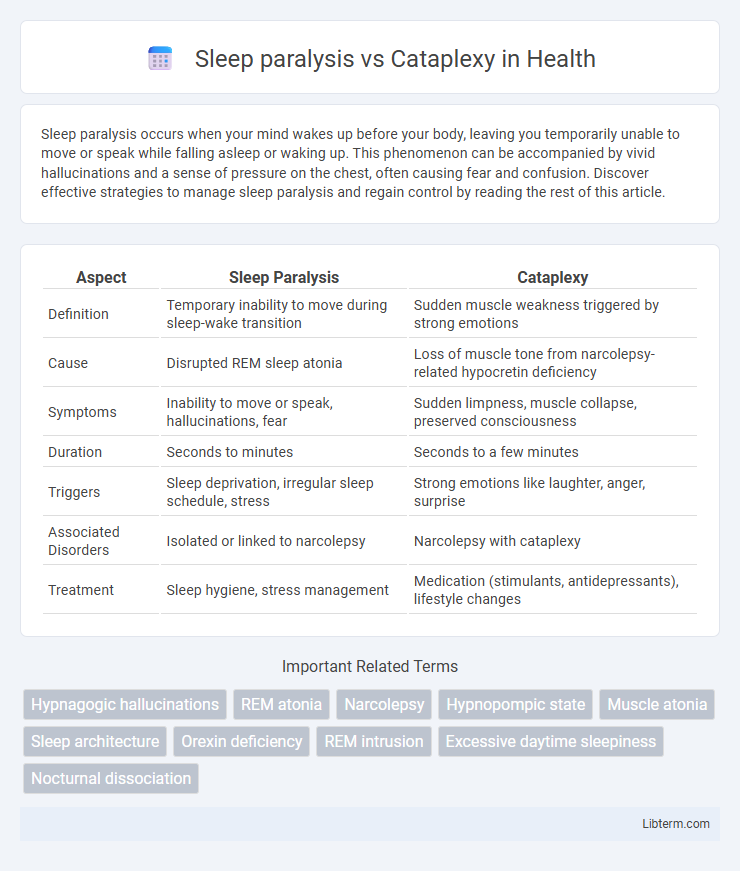
Table of Comparison
| Aspect | Sleep Paralysis | Cataplexy |
|---|---|---|
| Definition | Temporary inability to move during sleep-wake transition | Sudden muscle weakness triggered by strong emotions |
| Cause | Disrupted REM sleep atonia | Loss of muscle tone from narcolepsy-related hypocretin deficiency |
| Symptoms | Inability to move or speak, hallucinations, fear | Sudden limpness, muscle collapse, preserved consciousness |
| Duration | Seconds to minutes | Seconds to a few minutes |
| Triggers | Sleep deprivation, irregular sleep schedule, stress | Strong emotions like laughter, anger, surprise |
| Associated Disorders | Isolated or linked to narcolepsy | Narcolepsy with cataplexy |
| Treatment | Sleep hygiene, stress management | Medication (stimulants, antidepressants), lifestyle changes |
Understanding Sleep Paralysis
Sleep paralysis occurs when the brain awakens from REM sleep while the body remains temporarily immobile, causing an inability to move or speak despite full consciousness. It often includes hallucinations and a sense of pressure on the chest, which distinguishes it from cataplexy, a sudden, brief loss of muscle tone triggered by strong emotions in individuals with narcolepsy. Understanding sleep paralysis involves recognizing its connection to disrupted REM sleep cycles and differentiating it from neurological conditions like cataplexy for accurate diagnosis and treatment.
What is Cataplexy?
Cataplexy is a sudden and temporary muscle weakness often triggered by strong emotions such as laughter, anger, or surprise, commonly associated with narcolepsy. Unlike sleep paralysis, which occurs during the transition between sleep and wakefulness and involves an inability to move while conscious, cataplexy causes a brief loss of voluntary muscle control without loss of consciousness. Understanding cataplexy is crucial for diagnosing narcolepsy and differentiating it from other sleep disorders like sleep paralysis.
Key Differences Between Sleep Paralysis and Cataplexy
Sleep paralysis is characterized by temporary inability to move or speak while falling asleep or waking, often accompanied by vivid hallucinations. Cataplexy involves sudden muscle weakness triggered by strong emotions such as laughter or surprise, typically occurring during wakefulness in individuals with narcolepsy. Unlike sleep paralysis, cataplexy does not cause loss of consciousness and usually lasts seconds to minutes without hallucinations.
Causes of Sleep Paralysis
Sleep paralysis occurs when the brain transitions between sleep stages, causing temporary muscle atonia while consciousness is retained, often triggered by factors like sleep deprivation, irregular sleep schedules, stress, or narcolepsy. Cataplexy, distinctly linked to narcolepsy type 1, results from sudden muscle weakness triggered by strong emotions due to hypocretin deficiency in the brain. Understanding that sleep paralysis involves disrupted REM sleep atonia control helps differentiate it from cataplexy's emotional stimulus-induced muscle loss.
Causes of Cataplexy
Cataplexy is primarily caused by the loss of hypocretin-producing neurons in the hypothalamus, often linked to autoimmune mechanisms, whereas sleep paralysis results from the brain's inability to transition smoothly between REM sleep and wakefulness. The deficiency of hypocretin disrupts the regulation of muscle tone, leading to sudden muscle weakness triggered by strong emotions in cataplexy. Understanding these distinct neurological pathways is crucial for differentiating cataplexy from sleep paralysis and targeting appropriate treatments.
Symptoms Comparison: Sleep Paralysis vs Cataplexy
Sleep paralysis involves temporary inability to move or speak while falling asleep or waking, often accompanied by hallucinations and a sense of pressure on the chest. Cataplexy is characterized by sudden muscle weakness triggered by strong emotions such as laughter or surprise, without loss of consciousness. Unlike sleep paralysis, cataplexy episodes are brief, last seconds to minutes, and typically occur during wakefulness rather than during transitions in sleep.
Risk Factors and Triggers
Sleep paralysis risk factors include sleep deprivation, irregular sleep schedules, stress, and narcolepsy, while triggers often involve sudden awakenings and sleeping on the back. Cataplexy is primarily triggered by strong emotions such as laughter, anger, or surprise and is strongly associated with narcolepsy type 1 due to hypocretin deficiency. Both conditions share a genetic predisposition but differ in their physiological mechanisms and typical triggers.
Diagnosis and Recognition
Sleep paralysis is diagnosed primarily through patient history emphasizing episodes of temporary inability to move during sleep-wake transitions, often accompanied by hallucinations. Cataplexy diagnosis involves identifying sudden muscle weakness triggered by strong emotions, commonly confirmed via polysomnography combined with multiple sleep latency tests (MSLT) and observation of specific genetic markers like HLA-DQB1*06:02. Differentiating these disorders requires detailed clinical evaluation of episode triggers, duration, and associated symptoms to ensure accurate recognition and appropriate treatment planning.
Treatment Options for Each Condition
Treatment options for sleep paralysis primarily involve improving sleep hygiene, managing stress, and sometimes using medications such as antidepressants to regulate REM sleep. Cataplexy, often associated with narcolepsy, is treated with sodium oxybate, antidepressants like SSRIs or SNRIs, and lifestyle adjustments to avoid triggers. Both conditions benefit from a tailored approach by a sleep specialist to optimize symptom control and improve quality of life.
Preventive Strategies and Lifestyle Tips
Sleep paralysis prevention involves maintaining consistent sleep schedules, reducing stress, and avoiding sleep deprivation to promote healthy REM sleep cycles. Cataplexy management emphasizes triggers avoidance such as sudden emotions or stress, alongside prescribed medications like sodium oxybate or antidepressants to reduce episodes. Both conditions benefit from regular exercise, a balanced diet, and a calming pre-sleep routine to support overall neurological and sleep health.
Sleep paralysis Infographic
 libterm.com
libterm.com