Lipedema is a chronic disorder characterized by abnormal fat accumulation, primarily in the legs and arms, causing pain and swelling that can impact mobility. This condition often leads to easy bruising and sensitivity, distinguishing it from general obesity or lymphedema. Explore the rest of this article to understand Lipedema's symptoms, diagnosis, and effective treatment options tailored for your needs.
Table of Comparison
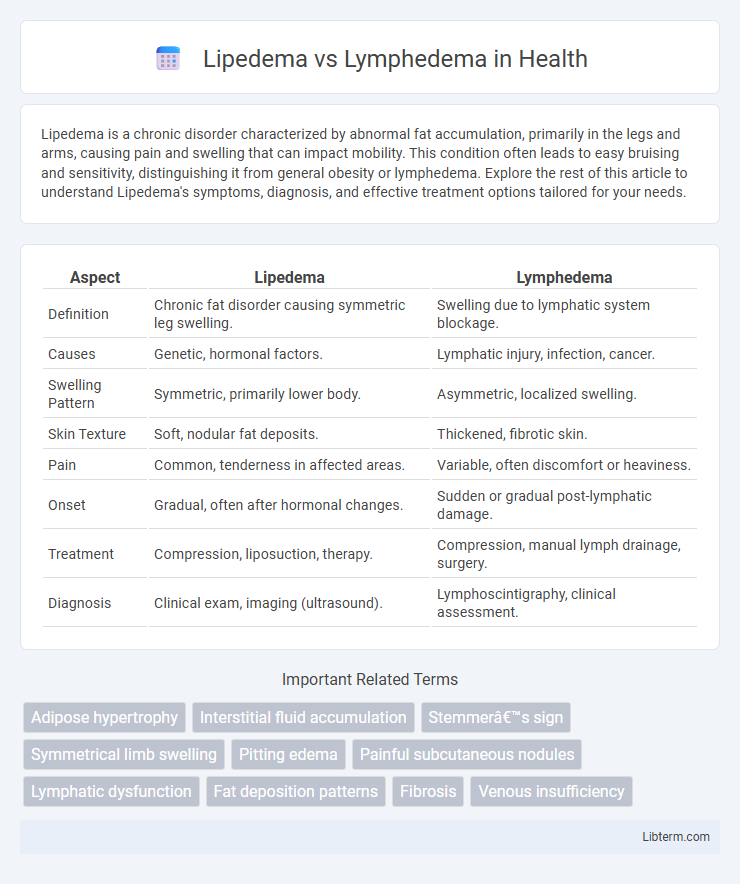
| Aspect | Lipedema | Lymphedema |
|---|---|---|
| Definition | Chronic fat disorder causing symmetric leg swelling. | Swelling due to lymphatic system blockage. |
| Causes | Genetic, hormonal factors. | Lymphatic injury, infection, cancer. |
| Swelling Pattern | Symmetric, primarily lower body. | Asymmetric, localized swelling. |
| Skin Texture | Soft, nodular fat deposits. | Thickened, fibrotic skin. |
| Pain | Common, tenderness in affected areas. | Variable, often discomfort or heaviness. |
| Onset | Gradual, often after hormonal changes. | Sudden or gradual post-lymphatic damage. |
| Treatment | Compression, liposuction, therapy. | Compression, manual lymph drainage, surgery. |
| Diagnosis | Clinical exam, imaging (ultrasound). | Lymphoscintigraphy, clinical assessment. |
Understanding Lipedema: Definition and Key Features
Lipedema is a chronic disorder characterized by the symmetrical accumulation of painful fat tissue, primarily affecting the legs and sometimes the arms, distinct from obesity and resistant to diet or exercise. Key features include easy bruising, sensitivity to touch, and a clear disproportion between the upper body and lower extremities, often resulting in a column-like leg shape. Unlike lymphedema, which involves lymphatic fluid buildup causing swelling, lipedema is a fat disorder with underlying hormonal and genetic influences.
What is Lymphedema? Causes and Characteristics
Lymphedema is a chronic condition characterized by the accumulation of lymphatic fluid, leading to swelling typically in the arms or legs, caused by damage or blockage in the lymphatic system. Common causes include lymph node removal, radiation therapy, infections, or congenital abnormalities that impair lymphatic drainage. Key characteristics involve persistent limb swelling, skin thickening, and increased risk of infections such as cellulitis due to compromised lymphatic function.
Core Differences Between Lipedema and Lymphedema
Lipedema primarily affects subcutaneous fat in the legs and sometimes arms, causing symmetrical swelling and pain, whereas lymphedema results from lymphatic system damage leading to fluid retention and swelling usually in one limb. Lipedema is characterized by disproportionate fat deposits that resist diet and exercise, while lymphedema involves chronic inflammation and skin changes due to lymph fluid accumulation. Diagnostic distinctions include lipedema's tenderness and bruising without pitting edema, contrasting with lymphedema's firm, pitting swelling and increased risk of infection.
Common Symptoms: How to Recognize Each Condition
Lipedema typically presents with symmetrical, painful fat accumulation in the legs and buttocks, often sparing the feet, accompanied by easy bruising and sensitivity. Lymphedema is characterized by unilateral or bilateral swelling caused by lymphatic fluid retention, primarily affecting the feet and progressing to the limbs with a feeling of heaviness and restricted mobility. Recognizing the distinction involves noting lipedema's disproportionate fat deposits and pain versus lymphedema's pitting edema and skin changes such as fibrosis and infections.
Causes and Risk Factors: Lipedema vs Lymphedema
Lipedema is caused by abnormal fat accumulation predominantly in the lower body, influenced by hormonal changes, genetics, and primarily affects women, while lymphedema results from lymphatic system damage or blockage, often due to surgery, infection, or radiation therapy. Risk factors for lipedema include family history and hormonal fluctuations during puberty, pregnancy, or menopause, whereas lymphedema risk increases with cancer treatments, chronic infections, and obesity. Both conditions involve swelling but differ fundamentally in pathophysiology, with lipedema linked to adipose tissue dysfunction and lymphedema to impaired lymphatic drainage.
Diagnostic Methods for Lipedema and Lymphedema
Diagnostic methods for lipedema primarily include clinical assessment through patient history and physical examination, emphasizing symmetrical fat distribution, pain, and easy bruising predominantly in the lower limbs. Lymphedema diagnosis often relies on imaging techniques such as lymphoscintigraphy, MRI, and ultrasound to detect lymphatic system dysfunction and swelling asymmetry. Both conditions may benefit from bioimpedance spectroscopy to differentiate fluid accumulation in lymphedema from adipose tissue proliferation characteristic of lipedema.
Stages and Progression of Each Disorder
Lipedema progresses through three clinically recognized stages characterized by increasing enlargement and nodularity of fatty tissue, primarily affecting the legs and sometimes arms, with stage one presenting smooth skin and stage three showing large lobules causing mobility issues. Lymphedema develops in four stages, from stage 0 (latent phase with no visible swelling) to stage 3 (elephantiasis), marked by severe swelling, skin changes, and fibrosis due to lymphatic system dysfunction. Both disorders exhibit progressive tissue changes, but lipedema is confined to subcutaneous fat with symmetrical distribution, whereas lymphedema involves lymph fluid accumulation leading to asymmetrical swelling and skin hardening.
Treatment Options: Comparing Therapies and Management
Lipedema treatment primarily involves conservative therapies such as compression garments, manual lymphatic drainage, and specialized exercise to reduce pain and swelling, with liposuction considered for advanced cases. Lymphedema management emphasizes meticulous skin care, complete decongestive therapy (CDT) including compression bandaging, manual lymphatic drainage, and pneumatic compression devices to improve lymphatic flow and prevent infections. Surgical options like lymphovenous bypass or vascularized lymph node transfer are more commonly applied in lymphedema due to structural lymphatic damage, whereas lipedema surgery focuses on fat removal while preserving lymphatic vessels.
Impact on Quality of Life and Daily Activities
Lipedema causes painful fat accumulation primarily in the legs and hips, leading to reduced mobility and chronic discomfort that significantly impairs daily activities and self-esteem. Lymphedema results from lymphatic fluid buildup causing persistent swelling, which can restrict movement, increase infection risk, and create challenges in performing routine tasks. Both conditions severely impact quality of life through physical limitations and emotional distress, necessitating targeted management strategies to improve patient outcomes.
When to Seek Medical Help: Early Intervention Tips
Persistent swelling in the legs, disproportionate fat accumulation, or pain that worsens with standing or sitting may indicate lipedema or lymphedema, necessitating early medical evaluation to prevent progression. Seek medical help if swelling is accompanied by skin changes such as redness, warmth, or ulcers, as these may signal complications like infections or lymphatic failure. Early intervention through specialized lymphatic therapy, compression garments, or lifestyle modifications greatly improves symptom management and quality of life in lipedema and lymphedema patients.
Lipedema Infographic
 libterm.com
libterm.com