Neutropenia is a condition characterized by an abnormally low level of neutrophils, a type of white blood cell essential for fighting infections. This decreases your body's ability to combat bacteria and fungi, leading to increased vulnerability to infections and requiring careful monitoring and treatment. Discover more about the causes, symptoms, and management strategies for neutropenia in the rest of this article.
Table of Comparison
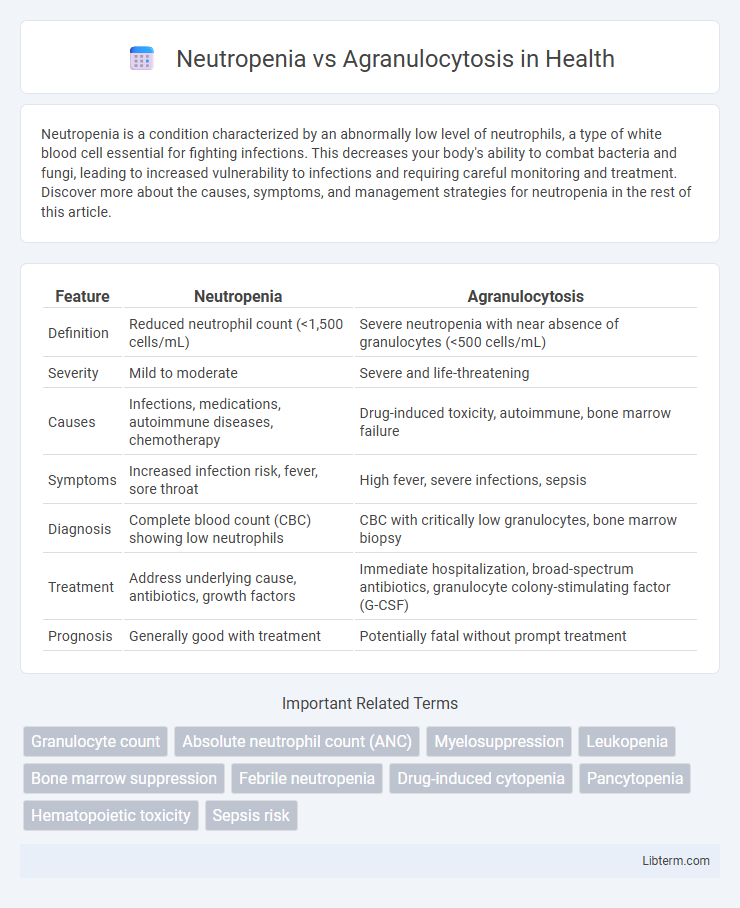
| Feature | Neutropenia | Agranulocytosis |
|---|---|---|
| Definition | Reduced neutrophil count (<1,500 cells/mL) | Severe neutropenia with near absence of granulocytes (<500 cells/mL) |
| Severity | Mild to moderate | Severe and life-threatening |
| Causes | Infections, medications, autoimmune diseases, chemotherapy | Drug-induced toxicity, autoimmune, bone marrow failure |
| Symptoms | Increased infection risk, fever, sore throat | High fever, severe infections, sepsis |
| Diagnosis | Complete blood count (CBC) showing low neutrophils | CBC with critically low granulocytes, bone marrow biopsy |
| Treatment | Address underlying cause, antibiotics, growth factors | Immediate hospitalization, broad-spectrum antibiotics, granulocyte colony-stimulating factor (G-CSF) |
| Prognosis | Generally good with treatment | Potentially fatal without prompt treatment |
Understanding Neutropenia and Agranulocytosis
Neutropenia is defined by an abnormally low count of neutrophils, a type of white blood cell essential for fighting infections, while agranulocytosis represents a severe form of neutropenia with an almost complete absence of granulocytes. Both conditions increase susceptibility to bacterial and fungal infections, but agranulocytosis presents a higher risk due to the drastic reduction in immune defense cells. Diagnosis typically involves a complete blood count (CBC) and bone marrow biopsy to determine the severity and underlying cause of granulocyte depletion.
Definitions and Key Differences
Neutropenia is defined as a reduced absolute neutrophil count (ANC) below 1,500 cells/uL, while agranulocytosis is a severe form of neutropenia with ANC less than 500 cells/uL, often leading to a near-complete absence of granulocytes. The key difference lies in severity and clinical risk; neutropenia can be mild, moderate, or severe, whereas agranulocytosis represents a critical depletion that significantly heightens the risk of infections. Both conditions involve impaired immune function but agranulocytosis requires urgent medical intervention due to its association with life-threatening complications.
Causes of Neutropenia
Neutropenia is primarily caused by bone marrow disorders, infections, autoimmune diseases, certain medications, and chemotherapy, which reduce neutrophil production or increase destruction. Agranulocytosis represents a severe form of neutropenia characterized by a near-complete absence of granulocytes, often linked to drug-induced toxicity or severe bone marrow suppression. Understanding these distinct causes is crucial for accurate diagnosis and targeted treatment strategies.
Causes of Agranulocytosis
Agranulocytosis primarily results from drug-induced bone marrow suppression, with common culprits including antithyroid medications, sulfonamides, and chemotherapy agents. Autoimmune disorders and severe infections can also lead to agranulocytosis by destroying granulocyte precursors. Unlike neutropenia, which broadly indicates low neutrophil counts from varied causes, agranulocytosis specifically refers to an almost complete absence of granulocytes, often triggered by toxic or immune-mediated bone marrow failure.
Risk Factors and Predisposing Conditions
Neutropenia commonly results from chemotherapy, autoimmune diseases, or viral infections, leading to a decreased neutrophil count and increased infection risk. Agranulocytosis, a severe form of neutropenia characterized by an almost complete absence of granulocytes, is often triggered by drug-induced toxicity, such as antithyroid medications, antibiotics, or anticonvulsants. Underlying conditions like bone marrow disorders, hematologic malignancies, or severe infections further predispose patients to both neutropenia and agranulocytosis.
Clinical Presentation and Symptoms
Neutropenia typically presents with mild or no symptoms but increases susceptibility to infections, evidenced by fever, sore throat, and oral ulcers. Agranulocytosis manifests more severely with sudden onset of high fever, chills, severe infections, and often painful ulcers in the mucous membranes due to an almost complete absence of neutrophils. Both conditions require prompt evaluation, but agranulocytosis poses a higher risk of life-threatening infections due to profound neutrophil depletion.
Diagnostic Criteria and Laboratory Findings
Neutropenia is defined by an absolute neutrophil count (ANC) below 1,500 cells/uL, while agranulocytosis refers to a severe form of neutropenia with ANC below 500 cells/uL, often indicating near-complete absence of granulocytes. Laboratory findings for neutropenia include decreased neutrophil counts on a complete blood count (CBC) with differential, whereas agranulocytosis shows a markedly reduced or absent granulocyte population, sometimes accompanied by bone marrow hypoplasia or aplasia on biopsy. Diagnostic criteria focus on ANC thresholds, clinical context, and exclusion of secondary causes such as infections or drug-induced marrow suppression.
Complications and Associated Risks
Neutropenia significantly increases the risk of bacterial and fungal infections due to a reduced neutrophil count, impairing the body's primary defense against pathogens. Agranulocytosis presents a more severe form of neutropenia, with an extremely low or near-absent granulocyte count, leading to life-threatening infections and sepsis risk. Both conditions require prompt management to prevent complications such as septic shock, but agranulocytosis demands immediate intervention because of its higher associated morbidity and mortality rates.
Treatment Strategies and Management
Neutropenia treatment strategies focus on preventing infections through prophylactic antibiotics, granulocyte colony-stimulating factor (G-CSF) administration, and close monitoring of neutrophil counts. Agranulocytosis management requires immediate cessation of causative agents, aggressive antimicrobial therapy, and supportive care, including hospitalization in severe cases. Both conditions necessitate tailored therapy based on severity and underlying causes to reduce infection risks and improve patient outcomes.
Prognosis and Prevention Strategies
Neutropenia, characterized by a low neutrophil count, generally has a better prognosis with timely treatment and avoidance of infectious complications, whereas agranulocytosis, signifying an almost complete absence of granulocytes, carries a higher risk of severe infections and poor outcomes if not promptly managed. Prevention strategies for neutropenia include regular monitoring of blood counts during chemotherapy and use of granulocyte colony-stimulating factors (G-CSF), while agranulocytosis prevention emphasizes identifying and discontinuing causative drugs and genetic screening for susceptibility in at-risk populations. Both conditions require strict infection control measures and patient education to reduce morbidity and improve overall prognosis.
Neutropenia Infographic
 libterm.com
libterm.com