Osteomalacia is a condition characterized by the softening of bones due to a deficiency in vitamin D, calcium, or phosphate, leading to bone pain and increased fracture risk. This disorder impairs bone mineralization, causing weakness and skeletal deformities that can significantly impact your mobility and quality of life. Explore the full article to understand the causes, symptoms, and effective treatments for osteomalacia.
Table of Comparison
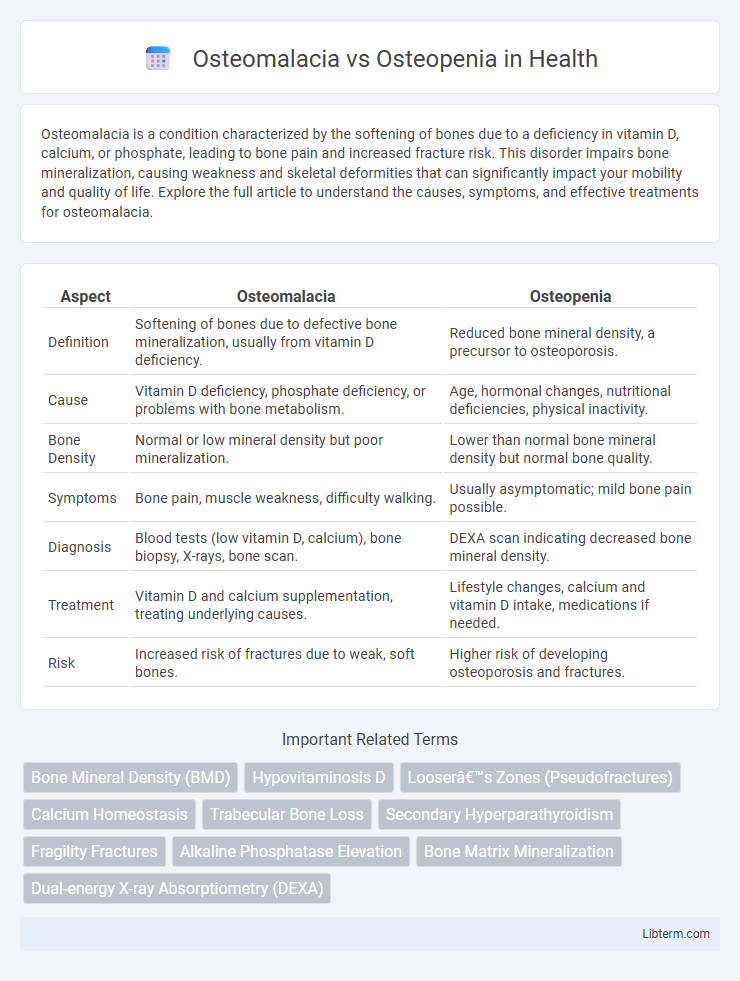
| Aspect | Osteomalacia | Osteopenia |
|---|---|---|
| Definition | Softening of bones due to defective bone mineralization, usually from vitamin D deficiency. | Reduced bone mineral density, a precursor to osteoporosis. |
| Cause | Vitamin D deficiency, phosphate deficiency, or problems with bone metabolism. | Age, hormonal changes, nutritional deficiencies, physical inactivity. |
| Bone Density | Normal or low mineral density but poor mineralization. | Lower than normal bone mineral density but normal bone quality. |
| Symptoms | Bone pain, muscle weakness, difficulty walking. | Usually asymptomatic; mild bone pain possible. |
| Diagnosis | Blood tests (low vitamin D, calcium), bone biopsy, X-rays, bone scan. | DEXA scan indicating decreased bone mineral density. |
| Treatment | Vitamin D and calcium supplementation, treating underlying causes. | Lifestyle changes, calcium and vitamin D intake, medications if needed. |
| Risk | Increased risk of fractures due to weak, soft bones. | Higher risk of developing osteoporosis and fractures. |
Introduction to Osteomalacia and Osteopenia
Osteomalacia is a metabolic bone disorder characterized by defective bone mineralization due to vitamin D deficiency, leading to soft, weak bones and increased fracture risk. Osteopenia refers to lower-than-normal bone mineral density (BMD) that is not severe enough to qualify as osteoporosis but indicates early bone loss. Both conditions compromise bone strength but differ fundamentally in etiology, with osteomalacia primarily involving impaired bone mineralization and osteopenia reflecting decreased bone mass.
Definitions: Osteomalacia vs Osteopenia
Osteomalacia is a bone disorder characterized by the softening of bones due to defective bone mineralization, primarily caused by vitamin D deficiency or phosphate metabolism abnormalities. Osteopenia refers to a condition where bone mineral density is lower than normal but not low enough to be classified as osteoporosis, indicating reduced bone strength and a higher risk of fractures. Both conditions affect bone health but differ in their underlying causes and the nature of bone deterioration.
Key Differences in Pathophysiology
Osteomalacia is characterized by defective bone mineralization due to vitamin D deficiency, leading to soft, weakened bones, while osteopenia involves decreased bone mineral density without a mineralization defect, often considered a precursor to osteoporosis. In osteomalacia, the impaired calcium and phosphate metabolism disrupts hydroxyapatite formation, causing accumulation of unmineralized osteoid. Osteopenia results mainly from an imbalance between bone resorption and formation, with normal mineralization but reduced bone mass and microarchitectural deterioration.
Causes and Risk Factors for Each Condition
Osteomalacia primarily results from vitamin D deficiency, leading to impaired bone mineralization and softening, with risk factors including malabsorption disorders, chronic kidney disease, and limited sunlight exposure. Osteopenia, characterized by reduced bone density preceding osteoporosis, is often caused by aging, hormonal changes such as decreased estrogen in postmenopausal women, and lifestyle factors like insufficient calcium intake, smoking, and sedentary behavior. Both conditions share risk factors like poor nutrition and certain medications but differ fundamentally in their pathological mechanisms and biochemical profiles.
Clinical Symptoms and Signs
Osteomalacia presents with diffuse bone pain, muscle weakness, and difficulty walking due to defective bone mineralization caused by vitamin D deficiency. Osteopenia is typically asymptomatic and identified through low bone mineral density on DEXA scans, without overt clinical signs. Unlike osteomalacia, osteopenia does not cause bone pain or muscle weakness but increases fracture risk due to decreased bone mass.
Diagnostic Criteria and Investigations
Osteomalacia is diagnosed through low serum calcium and phosphate levels, elevated alkaline phosphatase, and decreased vitamin D, confirmed by bone biopsy showing unmineralized osteoid; radiographs may reveal Looser's zones. Osteopenia is identified primarily by bone mineral density measurements using dual-energy X-ray absorptiometry (DEXA) with a T-score between -1.0 and -2.5, reflecting reduced bone mass but normal mineralization. Blood tests in osteopenia typically show normal calcium, phosphate, and alkaline phosphatase, differentiating it from the metabolic abnormalities seen in osteomalacia.
Treatments and Management Strategies
Osteomalacia treatment centers on correcting vitamin D deficiency through supplements and ensuring adequate calcium intake to restore bone mineralization, often requiring exposure to sunlight and addressing underlying causes like malabsorption. Osteopenia management emphasizes lifestyle changes such as weight-bearing exercises, smoking cessation, and dietary modifications with calcium and vitamin D to prevent progression to osteoporosis, sometimes supplemented by bisphosphonates or other osteoporosis medications. Both conditions benefit from regular bone density monitoring and tailored interventions to optimize bone health and reduce fracture risk.
Prognosis and Potential Complications
Osteomalacia typically presents with prolonged bone pain, muscle weakness, and an increased risk of fractures due to defective bone mineralization, often improving with vitamin D supplementation and proper treatment. Osteopenia indicates reduced bone density that may progress to osteoporosis, raising the risk of fractures but generally allowing for a favorable prognosis if addressed early with lifestyle changes and medication. Both conditions require ongoing monitoring to prevent complications such as pathological fractures and chronic skeletal deformities.
Prevention Tips for Bone Health
Maintaining adequate vitamin D and calcium intake is crucial for preventing both osteomalacia and osteopenia, as these nutrients support bone mineralization and density. Regular weight-bearing exercises like walking or resistance training help stimulate bone formation and reduce the risk of bone loss associated with these conditions. Avoiding smoking and excessive alcohol consumption further preserves bone health by minimizing factors that accelerate bone degradation.
Frequently Asked Questions (FAQs)
Osteomalacia is a bone-softening condition caused by vitamin D deficiency, leading to defective bone mineralization, while osteopenia involves reduced bone density that is less severe than osteoporosis but indicates bone weakening. Frequently asked questions include how to differentiate symptoms, with osteomalacia often presenting bone pain and muscle weakness, whereas osteopenia is usually asymptomatic and detected through bone density scans (DEXA). Treatment for osteomalacia focuses on vitamin D and calcium supplementation, whereas osteopenia management emphasizes lifestyle changes like diet, exercise, and sometimes medication to prevent progression to osteoporosis.
Osteomalacia Infographic
 libterm.com
libterm.com