Malignant conditions represent serious health threats due to their aggressive nature and potential to spread rapidly within the body. Early detection and effective treatment strategies are crucial to improving outcomes and managing symptoms. Explore the rest of the article to understand signs, treatments, and how you can support your health.
Table of Comparison
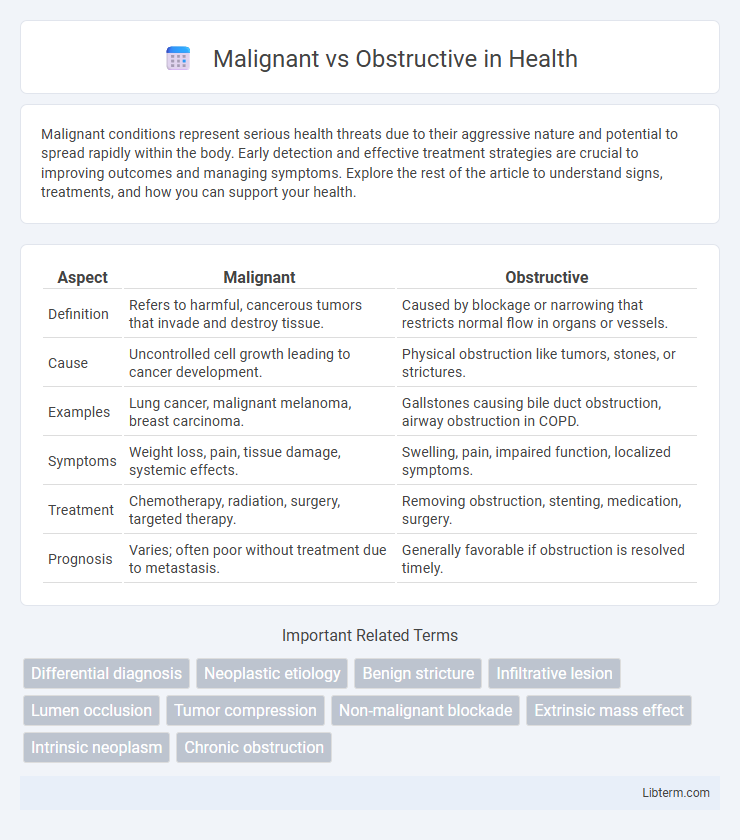
| Aspect | Malignant | Obstructive |
|---|---|---|
| Definition | Refers to harmful, cancerous tumors that invade and destroy tissue. | Caused by blockage or narrowing that restricts normal flow in organs or vessels. |
| Cause | Uncontrolled cell growth leading to cancer development. | Physical obstruction like tumors, stones, or strictures. |
| Examples | Lung cancer, malignant melanoma, breast carcinoma. | Gallstones causing bile duct obstruction, airway obstruction in COPD. |
| Symptoms | Weight loss, pain, tissue damage, systemic effects. | Swelling, pain, impaired function, localized symptoms. |
| Treatment | Chemotherapy, radiation, surgery, targeted therapy. | Removing obstruction, stenting, medication, surgery. |
| Prognosis | Varies; often poor without treatment due to metastasis. | Generally favorable if obstruction is resolved timely. |
Understanding Malignant vs Obstructive Conditions
Malignant conditions involve abnormal tissue growths typically associated with cancerous tumors that aggressively invade surrounding tissues and impair organ function. Obstructive conditions arise when normal physiological pathways are blocked, leading to impaired flow, such as in obstructive sleep apnea or urinary obstruction. Differentiating malignant from obstructive conditions requires diagnostic imaging, biopsy, and clinical evaluation to guide appropriate treatment strategies.
Key Definitions and Differences
Malignant obstruction refers to blockages caused by cancerous tumors that invade or compress organs and tissues, often leading to life-threatening complications. Obstructive conditions involve the physical blockage of a passageway, such as intestines or airways, which can result from benign causes like strictures, adhesions, or foreign bodies. Key differences lie in the etiology--malignant obstructions stem from neoplastic growths, whereas obstructive cases may arise from non-cancerous factors, influencing treatment options and prognosis significantly.
Causes of Malignant and Obstructive Disorders
Malignant disorders are primarily caused by uncontrolled cell growth due to genetic mutations, environmental factors such as carcinogen exposure, and viral infections like HPV or hepatitis B. Obstructive disorders result from structural blockages caused by physical factors like tumors, inflammation, or congenital abnormalities, leading to impaired flow in organs such as airways, blood vessels, or intestines. Understanding these distinct etiologies is critical for accurate diagnosis and targeted treatment strategies in malignant and obstructive diseases.
Common Symptoms to Watch For
Common symptoms of malignant and obstructive conditions often overlap but can indicate different underlying causes requiring distinct interventions. Malignant symptoms typically include unexplained weight loss, persistent pain, and rapidly growing masses, while obstructive symptoms often manifest as difficulty breathing, persistent cough, and localized swelling due to blockage. Recognizing signs such as hemoptysis, unexplained fatigue, and changes in organ function can aid in early differentiation and timely diagnosis.
Diagnostic Approaches and Tools
Diagnostic approaches for malignant airway obstruction often include imaging techniques such as computed tomography (CT) scans and positron emission tomography (PET) scans to identify tumor location, size, and metastasis. Bronchoscopy enables direct visualization and biopsy of suspicious lesions, providing histopathological confirmation essential for malignancy diagnosis. In contrast, obstructive airway conditions typically utilize spirometry and pulmonary function tests (PFTs) to assess airflow limitation, while imaging studies help detect causes like strictures or foreign bodies without tumor evidence.
Risk Factors and Patient Profiles
Malignant obstruction is commonly associated with advanced cancers such as pancreatic, colorectal, or lung tumors, presenting higher risk in older adults with a history of smoking, chronic inflammation, or genetic predispositions to malignancies. Obstructive conditions typically arise from benign causes like gallstones, strictures, or adhesions following surgery, more frequently seen in middle-aged patients with prior abdominal surgeries or inflammatory diseases such as Crohn's. Patient profiles for malignant obstruction often include rapid symptom progression and weight loss, whereas obstructive cases usually exhibit intermittent pain and a history of recurrent infections or biliary colic.
Treatment Strategies: Malignant vs Obstructive
Treatment strategies for malignant obstructions prioritize palliative measures such as stent placement, chemotherapy, and radiation therapy to manage tumor growth and alleviate symptoms. Obstructive conditions typically require surgical intervention or endoscopic procedures to remove or bypass blockages, focusing on restoring normal function. Selecting an approach depends on etiology, patient health status, and prognosis to optimize clinical outcomes and quality of life.
Prognosis and Outcomes Comparison
Malignant obstructions typically have a poorer prognosis due to the aggressive nature of underlying cancers and limited treatment options, often resulting in lower survival rates and increased complications. In contrast, benign obstructive causes usually allow for more favorable outcomes with timely intervention, including surgical or endoscopic procedures that can fully resolve the obstruction. Patient survival and quality of life dramatically improve when obstructions are managed promptly, emphasizing the importance of accurate diagnosis to distinguish malignant from benign causes.
Complications and Associated Risks
Malignant biliary obstruction often leads to complications such as cholangitis, hepatic abscesses, and progressive liver failure due to tumor growth and bile duct infiltration. Obstructive causes, typically benign like choledocholithiasis or strictures, are associated with risks including recurrent infections, biliary cirrhosis, and pancreatitis caused by impaired bile flow. Both conditions necessitate timely diagnosis and management to prevent irreversible liver damage and systemic complications.
Preventive Measures and Early Detection
Malignant strictures require regular screening with imaging techniques like CT scans and endoscopic ultrasound to enable early detection and timely intervention, often involving biopsy for histopathological confirmation. Preventive measures target risk factors such as smoking cessation, reducing exposure to carcinogens, and managing chronic inflammatory conditions like pancreatitis that predispose to malignant changes. Obstructive strictures benefit from early diagnosis through non-invasive tests like MRCP and symptom monitoring, with preventive strategies focusing on avoiding gallstone formation and treating benign causes promptly to prevent progression.
Malignant Infographic
 libterm.com
libterm.com