Pneumocystis pneumonia is a serious fungal infection primarily affecting individuals with weakened immune systems, leading to symptoms like fever, cough, and difficulty breathing. Early diagnosis and treatment are crucial to prevent severe respiratory complications. Discover essential information about risk factors, diagnosis, and effective treatment options to protect your health.
Table of Comparison
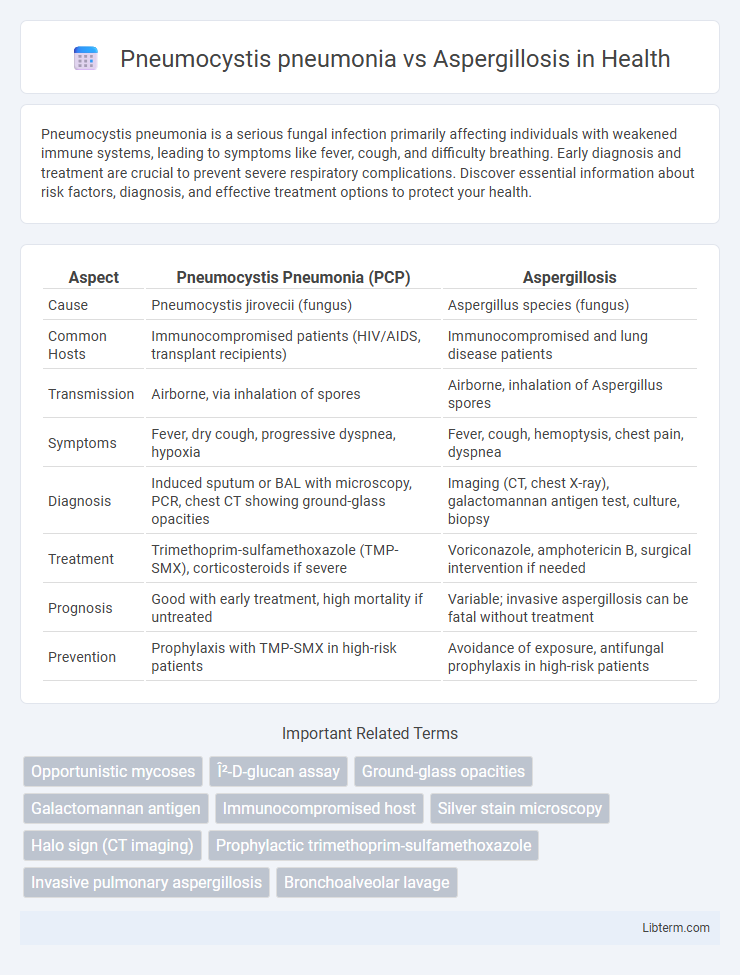
| Aspect | Pneumocystis Pneumonia (PCP) | Aspergillosis |
|---|---|---|
| Cause | Pneumocystis jirovecii (fungus) | Aspergillus species (fungus) |
| Common Hosts | Immunocompromised patients (HIV/AIDS, transplant recipients) | Immunocompromised and lung disease patients |
| Transmission | Airborne, via inhalation of spores | Airborne, inhalation of Aspergillus spores |
| Symptoms | Fever, dry cough, progressive dyspnea, hypoxia | Fever, cough, hemoptysis, chest pain, dyspnea |
| Diagnosis | Induced sputum or BAL with microscopy, PCR, chest CT showing ground-glass opacities | Imaging (CT, chest X-ray), galactomannan antigen test, culture, biopsy |
| Treatment | Trimethoprim-sulfamethoxazole (TMP-SMX), corticosteroids if severe | Voriconazole, amphotericin B, surgical intervention if needed |
| Prognosis | Good with early treatment, high mortality if untreated | Variable; invasive aspergillosis can be fatal without treatment |
| Prevention | Prophylaxis with TMP-SMX in high-risk patients | Avoidance of exposure, antifungal prophylaxis in high-risk patients |
Overview: Pneumocystis Pneumonia vs Aspergillosis
Pneumocystis pneumonia (PCP) is primarily caused by the fungal pathogen Pneumocystis jirovecii, leading to severe interstitial pneumonia in immunocompromised individuals, especially those with HIV/AIDS. Aspergillosis, caused by Aspergillus species, typically manifests as invasive pulmonary infection, allergic bronchopulmonary reactions, or chronic pulmonary aspergillosis, predominantly affecting patients with neutropenia, chronic lung diseases, or immunosuppression. Both infections require distinct diagnostic approaches and antifungal therapies, highlighting the importance of accurate identification and risk factor assessment in clinical management.
Causative Organisms: Pneumocystis jirovecii and Aspergillus Species
Pneumocystis pneumonia is caused by Pneumocystis jirovecii, a fungal organism primarily affecting immunocompromised patients, especially those with HIV/AIDS. Aspergillosis is caused by Aspergillus species, most commonly Aspergillus fumigatus, and typically affects individuals with weakened immune systems or underlying lung diseases. Both infections involve opportunistic fungi but differ significantly in their morphologies, environmental reservoirs, and typical clinical presentations.
Epidemiology and Risk Factors
Pneumocystis pneumonia (PCP) primarily affects immunocompromised individuals, such as those with HIV/AIDS, cancer patients undergoing chemotherapy, or organ transplant recipients, with an incidence peak in these populations globally. Aspergillosis is caused by Aspergillus species, predominantly affecting patients with prolonged neutropenia, chronic granulomatous disease, or severe immunosuppression, especially in hospital settings with airborne fungal spores. Both infections show increased prevalence in immunosuppressed hosts, but Aspergillosis also poses a significant risk in patients with underlying lung diseases such as chronic obstructive pulmonary disease (COPD) or cystic fibrosis.
Pathophysiology and Disease Progression
Pneumocystis pneumonia (PCP) is caused by the fungal pathogen Pneumocystis jirovecii, which primarily infects alveolar spaces, leading to diffuse interstitial pneumonia with alveolar damage and impaired gas exchange. Aspergillosis, caused by Aspergillus species, typically invades pulmonary tissue through hyphal growth, leading to angioinvasion, tissue necrosis, and formation of invasive or chronic pulmonary lesions. Disease progression in PCP involves widespread alveolar inflammation and collapse, often in immunocompromised patients, whereas aspergillosis progresses through tissue invasion and necrosis, potentially causing severe hemorrhage and systemic dissemination.
Clinical Manifestations: Similarities and Differences
Pneumocystis pneumonia (PCP) and Aspergillosis both present with respiratory symptoms such as cough, dyspnea, and fever, predominantly in immunocompromised patients. PCP often shows diffuse bilateral interstitial infiltrates on chest imaging, whereas Aspergillosis may exhibit nodules with halo signs or cavitary lesions. Hypoxemia is more pronounced in PCP, while Aspergillosis tends to involve airway invasion and hemoptysis.
Diagnostic Approaches: Imaging and Laboratory Tests
Pneumocystis pneumonia (PCP) diagnosis often relies on high-resolution computed tomography (HRCT) revealing bilateral ground-glass opacities, while Aspergillosis typically presents with nodules, cavitation, or halo signs on chest CT scans. Laboratory tests for PCP include identification of Pneumocystis jirovecii DNA by polymerase chain reaction (PCR) from bronchoalveolar lavage (BAL) fluid and elevated serum beta-D-glucan levels. In Aspergillosis, detection of galactomannan antigen in serum or BAL fluid and culture or PCR assays confirming Aspergillus species are critical for diagnosis.
Treatment Strategies: Antifungals and Supportive Care
Pneumocystis pneumonia (PCP) treatment primarily involves high-dose Trimethoprim-sulfamethoxazole (TMP-SMX) combined with corticosteroids for patients with moderate-to-severe disease to reduce inflammation. Aspergillosis management relies on antifungal agents such as voriconazole or isavuconazole, with amphotericin B reserved for refractory cases. Supportive care for both infections includes oxygen therapy and mechanical ventilation when respiratory failure develops, emphasizing the need for early diagnosis and tailored antifungal regimens to improve patient outcomes.
Prognosis and Outcomes
Pneumocystis pneumonia (PCP) primarily affects immunocompromised individuals and has a variable prognosis, with early diagnosis and treatment significantly improving survival rates to around 70-90%. Aspergillosis, particularly invasive aspergillosis, carries a poorer prognosis, with mortality rates exceeding 50% in immunosuppressed patients despite antifungal therapy. Outcomes for both infections depend heavily on the patient's immune status and timely initiation of appropriate antimicrobial or antifungal treatment.
Prevention and Prophylaxis Measures
Pneumocystis pneumonia prevention primarily involves prophylactic use of trimethoprim-sulfamethoxazole in immunocompromised patients, especially those with HIV/AIDS or undergoing chemotherapy. Aspergillosis prevention focuses on minimizing exposure to Aspergillus spores through environmental controls such as HEPA filtration and avoidance of construction areas for high-risk patients. Both infections require tailored antifungal or antimicrobial prophylaxis based on individual risk factors and immune status to effectively reduce incidence.
Key Takeaways and Clinical Implications
Pneumocystis pneumonia (PCP) primarily affects immunocompromised patients, especially those with HIV/AIDS, presenting with subacute respiratory symptoms and characteristic bilateral interstitial infiltrates on imaging. Aspergillosis, caused by Aspergillus species, manifests in diverse forms including invasive pulmonary aspergillosis in neutropenic or severely immunosuppressed patients, often showing nodular lesions with halo signs on CT scans. Prompt differentiation using specific diagnostic tools such as PCR, galactomannan assay for Aspergillus, and induced sputum or bronchoalveolar lavage for Pneumocystis is critical for targeted antifungal therapy and improved clinical outcomes.
Pneumocystis pneumonia Infographic
 libterm.com
libterm.com