Hyponatremia occurs when sodium levels in the blood drop below normal, disrupting the balance of fluids in your body and leading to symptoms like headache, confusion, and fatigue. Causes range from dehydration and excessive fluid intake to underlying medical conditions such as heart failure or kidney disease. Discover more about hyponatremia's symptoms, causes, and treatments in the full article.
Table of Comparison
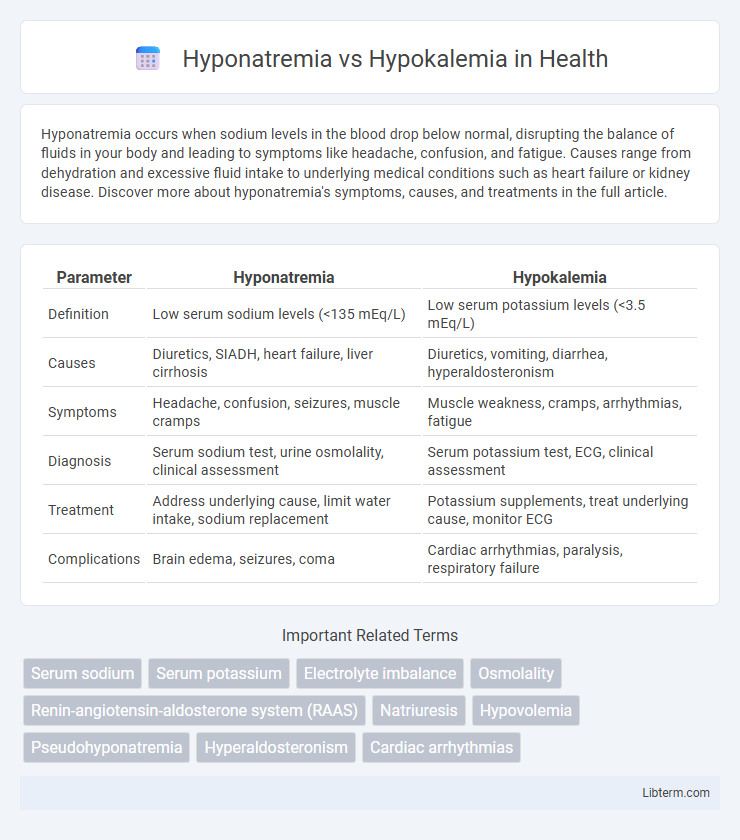
| Parameter | Hyponatremia | Hypokalemia |
|---|---|---|
| Definition | Low serum sodium levels (<135 mEq/L) | Low serum potassium levels (<3.5 mEq/L) |
| Causes | Diuretics, SIADH, heart failure, liver cirrhosis | Diuretics, vomiting, diarrhea, hyperaldosteronism |
| Symptoms | Headache, confusion, seizures, muscle cramps | Muscle weakness, cramps, arrhythmias, fatigue |
| Diagnosis | Serum sodium test, urine osmolality, clinical assessment | Serum potassium test, ECG, clinical assessment |
| Treatment | Address underlying cause, limit water intake, sodium replacement | Potassium supplements, treat underlying cause, monitor ECG |
| Complications | Brain edema, seizures, coma | Cardiac arrhythmias, paralysis, respiratory failure |
Introduction to Hyponatremia and Hypokalemia
Hyponatremia is characterized by abnormally low sodium levels in the blood, typically below 135 mEq/L, leading to symptoms like headache, confusion, and seizures due to cellular swelling. Hypokalemia refers to a potassium deficiency in the bloodstream, with levels under 3.5 mEq/L, causing muscle weakness, cramps, and cardiac arrhythmias due to impaired cellular function. Both electrolyte imbalances require prompt diagnosis and management to prevent severe neurological and cardiovascular complications.
Definitions and Key Differences
Hyponatremia is defined by a serum sodium concentration below 135 mEq/L, primarily affecting extracellular fluid balance and leading to symptoms like headache, nausea, and confusion. Hypokalemia occurs when serum potassium levels fall below 3.5 mEq/L, impacting cellular function and muscle contraction, often causing weakness, cramps, and cardiac arrhythmias. The key difference lies in their electrolyte imbalance: hyponatremia involves sodium depletion affecting fluid regulation, whereas hypokalemia involves potassium deficiency impacting cardiac and neuromuscular function.
Causes of Hyponatremia
Hyponatremia primarily results from conditions that cause an excess of water relative to sodium, including heart failure, liver cirrhosis, and the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Other common causes include diuretic use, adrenal insufficiency, and chronic kidney disease, which impair sodium balance and fluid regulation. Understanding the underlying etiology is critical for accurately diagnosing and managing hyponatremia in clinical practice.
Causes of Hypokalemia
Hypokalemia, characterized by low serum potassium levels, commonly results from factors such as excessive potassium loss through gastrointestinal routes like vomiting or diarrhea, diuretic use increasing renal potassium excretion, and conditions like hyperaldosteronism promoting renal potassium wasting. In contrast, hyponatremia arises primarily from an imbalance in sodium and water homeostasis, often due to conditions like syndrome of inappropriate antidiuretic hormone secretion (SIADH), heart failure, or renal disease. Understanding the underlying causes of hypokalemia is critical for effective treatment and prevention of complications like cardiac arrhythmias and muscle weakness.
Clinical Manifestations
Hyponatremia presents primarily with neurological symptoms such as headache, confusion, seizures, and in severe cases, coma due to cerebral edema. Hypokalemia is characterized by muscle weakness, cramps, arrhythmias, and fatigue resulting from impaired muscle and cardiac cell function. Both electrolyte imbalances can cause profound effects on the nervous and muscular systems, requiring prompt diagnosis and management.
Diagnostic Approaches
Hyponatremia diagnosis centers on measuring serum sodium levels below 135 mEq/L, assessing serum osmolality, urine sodium concentration, and evaluating volume status to distinguish between causes such as hypovolemic, euvolemic, or hypervolemic states. Hypokalemia diagnosis requires confirming serum potassium levels below 3.5 mEq/L, along with ECG monitoring for characteristic changes like U waves, and assessing renal potassium excretion via urine potassium measurement to identify renal or extrarenal potassium losses. Both conditions benefit from detailed patient history, medication review, and evaluation of acid-base balance to guide targeted treatment strategies.
Treatment Strategies
Treatment strategies for hyponatremia primarily involve controlled sodium replacement through intravenous saline solutions and addressing underlying causes such as fluid overload or hormonal imbalances. Hypokalemia treatment focuses on potassium supplementation either orally or intravenously, combined with monitoring cardiac function and correcting contributing factors like diuretic use or gastrointestinal losses. Both conditions require careful electrolyte monitoring to avoid complications such as cardiac arrhythmias or neurological deficits.
Complications and Risks
Hyponatremia, characterized by low sodium levels, can lead to severe neurological complications such as cerebral edema, seizures, and in extreme cases, coma due to disrupted cellular homeostasis. Hypokalemia, marked by low potassium levels, poses significant cardiac risks including arrhythmias, muscle weakness, and paralysis, primarily affecting cardiac and muscular function. Both electrolyte imbalances require timely diagnosis and management to prevent potentially life-threatening outcomes related to heart and brain function.
Prevention and Management Tips
Preventing hyponatremia involves monitoring sodium intake and maintaining proper hydration, especially during prolonged exercise or illness that causes fluid loss. To manage hypokalemia, increasing dietary potassium through foods like bananas, oranges, and spinach and avoiding excessive diuretics are essential strategies. Regular blood tests and timely supplementation under medical guidance ensure effective control of both electrolyte imbalances and reduce the risk of complications.
Prognosis and Long-Term Outcomes
Hyponatremia prognosis depends heavily on the underlying cause, severity, and rate of sodium correction, with chronic mild cases often having favorable outcomes, while acute or severe hyponatremia can lead to neurological damage and increased mortality. Hypokalemia prognosis is generally positive if potassium levels are promptly restored, but severe or persistent hypokalemia may result in cardiac arrhythmias, muscle weakness, and long-term renal impairment. Long-term outcomes for both electrolyte imbalances improve significantly with early detection, proper management, and monitoring to prevent recurrent episodes and associated complications.
Hyponatremia Infographic
 libterm.com
libterm.com