Seizures occur due to abnormal electrical activity in the brain, leading to sudden and uncontrolled physical or behavioral changes. Recognizing different types of seizures and understanding their triggers can help you manage or seek timely treatment. Explore the rest of the article to learn more about symptoms, causes, and effective management strategies.
Table of Comparison
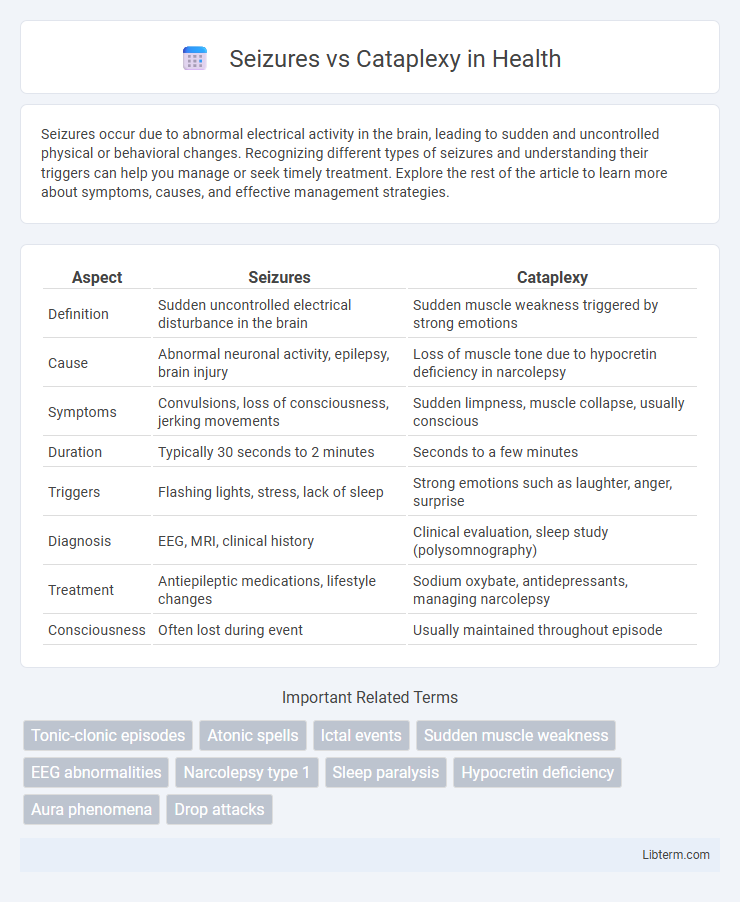
| Aspect | Seizures | Cataplexy |
|---|---|---|
| Definition | Sudden uncontrolled electrical disturbance in the brain | Sudden muscle weakness triggered by strong emotions |
| Cause | Abnormal neuronal activity, epilepsy, brain injury | Loss of muscle tone due to hypocretin deficiency in narcolepsy |
| Symptoms | Convulsions, loss of consciousness, jerking movements | Sudden limpness, muscle collapse, usually conscious |
| Duration | Typically 30 seconds to 2 minutes | Seconds to a few minutes |
| Triggers | Flashing lights, stress, lack of sleep | Strong emotions such as laughter, anger, surprise |
| Diagnosis | EEG, MRI, clinical history | Clinical evaluation, sleep study (polysomnography) |
| Treatment | Antiepileptic medications, lifestyle changes | Sodium oxybate, antidepressants, managing narcolepsy |
| Consciousness | Often lost during event | Usually maintained throughout episode |
Understanding Seizures: Definition and Causes
Seizures are sudden, uncontrolled electrical disturbances in the brain that can cause changes in behavior, movements, or consciousness. Common causes include epilepsy, brain injury, infections, genetic disorders, and metabolic imbalances such as low blood sugar or electrolyte abnormalities. Differentiating seizures from cataplexy is crucial, as seizures involve abnormal electrical activity, whereas cataplexy is a sudden loss of muscle tone triggered by strong emotions, often linked to narcolepsy.
What Is Cataplexy? Key Characteristics
Cataplexy is a sudden, brief loss of voluntary muscle tone triggered by strong emotions, such as laughter or surprise, typically lasting seconds to minutes without loss of consciousness. Unlike seizures, cataplexy does not involve abnormal electrical brain activity or convulsions but presents as muscle weakness or paralysis while the person remains fully aware. It is a hallmark symptom of narcolepsy type 1 and often coexists with excessive daytime sleepiness and disrupted nighttime sleep.
Symptoms: Seizures vs Cataplexy
Seizures present with sudden, uncontrolled electrical disturbances in the brain causing convulsions, loss of consciousness, or abnormal sensations, while cataplexy involves sudden muscle weakness triggered by strong emotions without loss of consciousness. Seizures may include symptoms such as jerking movements, staring spells, or confusion, contrasting with cataplexy's hallmark symptoms of brief episodes of muscle slackening, often affecting the face, neck, or limbs. Both conditions can appear similar but differ fundamentally in symptom triggers and neurological mechanisms.
Triggers and Risk Factors
Seizures are often triggered by factors such as sleep deprivation, stress, flashing lights, and fever, with risk factors including epilepsy, brain injury, and genetic predisposition. Cataplexy, a sudden loss of muscle tone triggered primarily by strong emotions like laughter, surprise, or anger, is strongly associated with narcolepsy type 1 and autoimmune dysfunction targeting hypocretin-producing neurons. Understanding these distinct triggers and risk factors is crucial for accurate diagnosis and effective management of each condition.
Neurological Mechanisms Compared
Seizures arise from abnormal, excessive electrical discharges in the brain's neurons, often linked to epilepsy or brain injury, disrupting normal neurological function. Cataplexy involves sudden, transient muscle weakness triggered by strong emotions, caused by the loss of hypocretin-producing neurons in the hypothalamus, which regulate muscle tone inhibition. While seizures reflect hyperexcitable neuronal activity, cataplexy results from dysregulation of sleep-wake mechanisms and selective muscle atonia.
Diagnostic Differences
Seizures and cataplexy differ significantly in diagnostic criteria, with seizures typically identified through electroencephalogram (EEG) abnormalities showing abnormal electrical brain activity. Cataplexy diagnosis relies primarily on clinical history and polysomnography (sleep study), often combined with a multiple sleep latency test (MSLT), to detect rapid eye movement (REM) sleep abnormalities and muscle tone loss during wakefulness. Unlike seizures, cataplexy episodes are triggered by strong emotions and lack the abnormal EEG findings characteristic of epileptic seizures.
Treatment Approaches for Seizures
Treatment approaches for seizures primarily involve antiepileptic drugs (AEDs) such as levetiracetam, valproate, and carbamazepine, which aim to reduce the frequency and severity of seizure episodes by stabilizing neuronal activity. In refractory cases, options include surgical interventions like resective surgery or neuromodulation techniques such as vagus nerve stimulation and responsive neurostimulation. Lifestyle modifications and seizure management plans tailored to the patient's specific seizure type and triggers are critical components of effective long-term seizure control.
Managing Cataplexy Episodes
Managing cataplexy episodes involves the use of prescription medications such as sodium oxybate and antidepressants like selective serotonin reuptake inhibitors (SSRIs) or tricyclic antidepressants to reduce symptom frequency and severity. Lifestyle adjustments, including avoiding known triggers such as sudden emotions or stress, play a critical role in minimizing episodes effectively. Regular consultation with a neurologist or sleep specialist helps tailor treatment plans and monitor progress in distinguishing cataplexy from seizures.
When to Seek Medical Attention
Seek medical attention immediately if seizures or cataplexy episodes occur with sudden loss of consciousness or prolonged muscle weakness. Seizures lasting longer than five minutes or repeated episodes without recovery require emergency care to prevent brain damage. Cataplexy causing frequent falls, difficulty breathing, or swallowing problems also warrants prompt evaluation by a healthcare professional.
Living with Seizures or Cataplexy: Tips and Support
Living with seizures or cataplexy requires careful management through medication adherence, avoiding known triggers, and maintaining a structured daily routine to minimize episodes. Accessing support groups and working closely with healthcare providers can provide emotional support and customized treatment plans to improve quality of life. Implementing safety measures at home and informing family, friends, and employers about the conditions ensures preparedness and reduces risks during episodes.
Seizures Infographic
 libterm.com
libterm.com