Subclinical hypothyroidism occurs when thyroid-stimulating hormone (TSH) levels are elevated but thyroid hormone levels remain normal, often causing subtle or no symptoms. This condition can impact metabolic health and requires careful diagnosis to distinguish it from overt hypothyroidism or other thyroid disorders. Discover more about the causes, symptoms, and treatment options to understand how your thyroid function may affect your overall well-being.
Table of Comparison
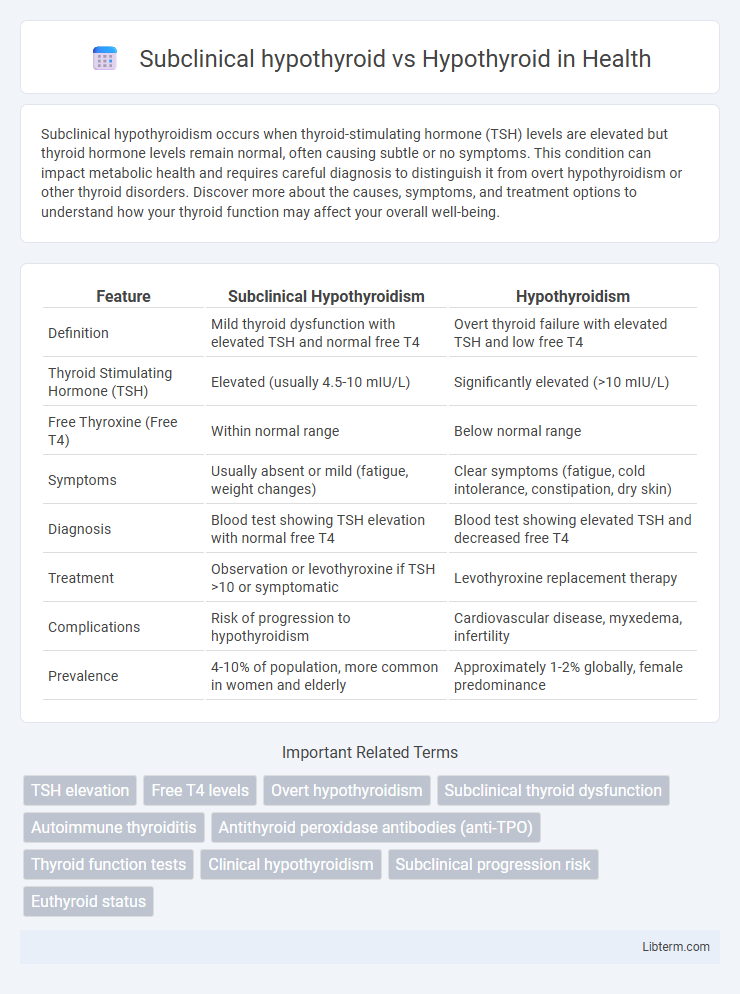
| Feature | Subclinical Hypothyroidism | Hypothyroidism |
|---|---|---|
| Definition | Mild thyroid dysfunction with elevated TSH and normal free T4 | Overt thyroid failure with elevated TSH and low free T4 |
| Thyroid Stimulating Hormone (TSH) | Elevated (usually 4.5-10 mIU/L) | Significantly elevated (>10 mIU/L) |
| Free Thyroxine (Free T4) | Within normal range | Below normal range |
| Symptoms | Usually absent or mild (fatigue, weight changes) | Clear symptoms (fatigue, cold intolerance, constipation, dry skin) |
| Diagnosis | Blood test showing TSH elevation with normal free T4 | Blood test showing elevated TSH and decreased free T4 |
| Treatment | Observation or levothyroxine if TSH >10 or symptomatic | Levothyroxine replacement therapy |
| Complications | Risk of progression to hypothyroidism | Cardiovascular disease, myxedema, infertility |
| Prevalence | 4-10% of population, more common in women and elderly | Approximately 1-2% globally, female predominance |
Understanding Hypothyroid and Subclinical Hypothyroid
Subclinical hypothyroidism is characterized by elevated thyroid-stimulating hormone (TSH) levels with normal free thyroxine (T4), often presenting minimal or no symptoms, while overt hypothyroidism involves elevated TSH and low T4 levels with clear clinical symptoms such as fatigue, weight gain, and cold intolerance. Understanding hypothyroidism requires recognizing that subclinical cases may progress to overt hypothyroidism, especially if TSH levels exceed 10 mIU/L or if thyroid autoantibodies are present. Early diagnosis through sensitive TSH testing and monitoring thyroid function can guide treatment decisions and prevent complications associated with untreated hypothyroidism.
Defining Subclinical Hypothyroidism
Subclinical hypothyroidism is characterized by elevated thyroid-stimulating hormone (TSH) levels with normal free thyroxine (T4) concentrations, distinguishing it from overt hypothyroidism, where both TSH is elevated and free T4 is decreased. This condition often presents without obvious clinical symptoms but may progress to hypothyroidism or affect cardiovascular health if untreated. Early detection through thyroid function tests enables timely management to prevent complications associated with thyroid hormone deficiency.
What Constitutes Overt Hypothyroidism?
Overt hypothyroidism is characterized by elevated serum thyroid-stimulating hormone (TSH) levels above the normal reference range, typically exceeding 10 mIU/L, alongside decreased free thyroxine (FT4) levels indicating insufficient thyroid hormone production. In contrast, subclinical hypothyroidism presents with elevated TSH but normal FT4 levels, reflecting early thyroid dysfunction without clear clinical symptoms. Diagnosis of overt hypothyroidism relies on biochemical evidence of both high TSH and low FT4, confirming a definitive thyroid hormone deficiency requiring treatment.
Key Differences: Subclinical vs. Overt Hypothyroidism
Subclinical hypothyroidism is characterized by elevated thyroid-stimulating hormone (TSH) levels with normal free thyroxine (T4) levels, indicating early or mild thyroid dysfunction, whereas overt hypothyroidism presents with both elevated TSH and low free T4 levels, reflecting significant thyroid hormone deficiency. Symptoms in subclinical hypothyroidism are often mild or absent, while overt hypothyroidism typically manifests with clear clinical signs like fatigue, weight gain, and cold intolerance. Diagnosis hinges on laboratory thyroid function tests with TSH as the primary marker, and treatment decisions differ: subclinical cases may require monitoring or low-dose levothyroxine, while overt hypothyroidism demands full replacement therapy.
Symptoms Comparison: Subclinical vs. Hypothyroid
Subclinical hypothyroidism often presents with subtle or no symptoms, making diagnosis reliant on elevated TSH levels with normal free T4, whereas overt hypothyroidism manifests clear symptoms such as fatigue, weight gain, cold intolerance, and constipation. Patients with hypothyroidism typically experience more pronounced symptoms due to significant thyroid hormone deficiency affecting metabolism and organ function. Early detection of subclinical hypothyroidism is crucial to monitor progression and prevent symptomatic hypothyroidism.
Causes and Risk Factors
Subclinical hypothyroidism is primarily caused by autoimmune thyroiditis, iodine deficiency, or mild thyroid hormone resistance, while overt hypothyroidism often results from Hashimoto's thyroiditis, thyroidectomy, or radioactive iodine treatment. Risk factors for subclinical hypothyroidism include female gender, advanced age, and family history of thyroid disease, whereas hypothyroidism risk factors also encompass iodine deficiency, certain medications such as lithium or amiodarone, and exposure to radiation. Both conditions share autoimmune disorders and genetic predispositions as significant underlying contributors.
Diagnostic Criteria and Laboratory Findings
Subclinical hypothyroidism is characterized by elevated thyroid-stimulating hormone (TSH) levels with normal free thyroxine (FT4) concentrations, whereas overt hypothyroidism presents with elevated TSH and decreased FT4 levels. Diagnostic criteria for subclinical hypothyroidism typically involve a TSH level above the upper laboratory reference limit (commonly 4.0-4.5 mIU/L) and normal FT4, while hypothyroidism diagnosis requires elevated TSH and low FT4 confirming thyroid hormone deficiency. Laboratory findings in hypothyroidism may also include positive anti-thyroid peroxidase (anti-TPO) antibodies, indicating autoimmune thyroiditis, which is often associated with both subclinical and overt hypothyroid states.
Management and Treatment Approaches
Subclinical hypothyroid is characterized by elevated TSH levels with normal free T4, often managed with regular monitoring and lifestyle modifications, reserving treatment for patients with TSH >10 mIU/L or symptomatic cases. Overt hypothyroid requires definitive levothyroxine replacement therapy to normalize thyroid hormone levels and alleviate symptoms, with dosage tailored to maintain TSH within the reference range. Both conditions benefit from regular thyroid function testing, but overt hypothyroid demands more aggressive and consistent treatment to prevent complications.
Prognosis and Long-term Outcomes
Subclinical hypothyroidism is characterized by elevated thyroid-stimulating hormone (TSH) levels with normal free thyroxine (T4), often presenting minimal or no symptoms and generally exhibiting a favorable prognosis with low risk of progression to overt hypothyroidism. In contrast, overt hypothyroidism involves both elevated TSH and low free T4, leading to significant clinical symptoms and a higher risk of cardiovascular complications, cognitive impairment, and decreased quality of life if untreated. Long-term outcomes of subclinical hypothyroidism vary based on TSH levels, patient age, and comorbidities, making monitoring essential, while untreated overt hypothyroidism typically requires lifelong thyroid hormone replacement to prevent severe morbidity.
Frequently Asked Questions
Subclinical hypothyroidism is characterized by elevated thyroid-stimulating hormone (TSH) levels with normal free thyroxine (T4), whereas overt hypothyroidism presents with high TSH and low T4 levels. Frequently asked questions often address symptoms differentiation, diagnosis criteria, and treatment options for both conditions, emphasizing blood test thresholds and potential progression risks. Patients commonly inquire about the necessity of levothyroxine therapy in subclinical cases and the impact on cardiovascular and metabolic health.
Subclinical hypothyroid Infographic
 libterm.com
libterm.com