Gallbladder disease encompasses various conditions affecting the gallbladder, such as gallstones, inflammation, and infections that cause pain and digestive issues. Early diagnosis and targeted treatment are crucial to prevent complications like bile duct obstruction or gallbladder rupture. Discover more about symptoms, causes, and effective management options in the rest of this article.
Table of Comparison
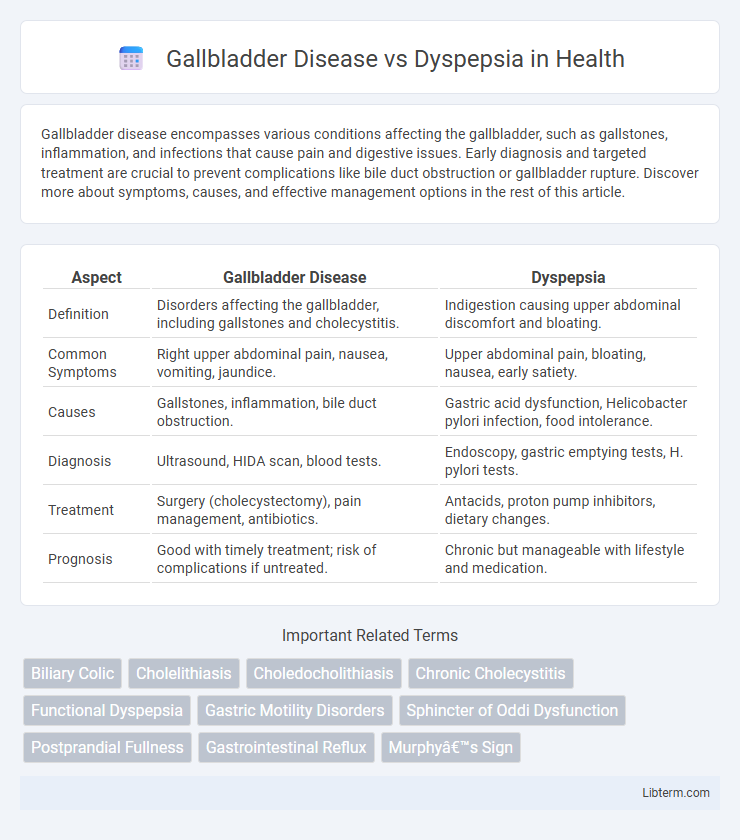
| Aspect | Gallbladder Disease | Dyspepsia |
|---|---|---|
| Definition | Disorders affecting the gallbladder, including gallstones and cholecystitis. | Indigestion causing upper abdominal discomfort and bloating. |
| Common Symptoms | Right upper abdominal pain, nausea, vomiting, jaundice. | Upper abdominal pain, bloating, nausea, early satiety. |
| Causes | Gallstones, inflammation, bile duct obstruction. | Gastric acid dysfunction, Helicobacter pylori infection, food intolerance. |
| Diagnosis | Ultrasound, HIDA scan, blood tests. | Endoscopy, gastric emptying tests, H. pylori tests. |
| Treatment | Surgery (cholecystectomy), pain management, antibiotics. | Antacids, proton pump inhibitors, dietary changes. |
| Prognosis | Good with timely treatment; risk of complications if untreated. | Chronic but manageable with lifestyle and medication. |
Introduction: Understanding Gallbladder Disease and Dyspepsia
Gallbladder disease encompasses conditions like gallstones and cholecystitis that impair bile storage and digestion, causing severe abdominal pain and digestive disturbances. Dyspepsia, often termed indigestion, manifests as upper abdominal discomfort, bloating, and nausea, typically linked to stomach acid imbalance or motility issues. Distinguishing between gallbladder disease and dyspepsia is critical for accurate diagnosis and effective treatment, as their symptoms frequently overlap but stem from different pathologies.
Definition and Overview of Gallbladder Disease
Gallbladder disease encompasses a range of conditions affecting the gallbladder, including gallstones, cholecystitis, and biliary dyskinesia, characterized by inflammation, pain, and digestion issues. Unlike dyspepsia, which manifests as general indigestion and upper abdominal discomfort without specific gallbladder pathology, gallbladder disease involves structural or functional abnormalities within the gallbladder itself. Early diagnosis of gallbladder disease is critical to prevent complications such as infection or bile duct obstruction.
Dyspepsia: Meaning and Common Causes
Dyspepsia, commonly known as indigestion, refers to a collection of symptoms including upper abdominal discomfort, bloating, nausea, and belching that affect digestion. Common causes of dyspepsia include gastroesophageal reflux disease (GERD), peptic ulcers, Helicobacter pylori infection, and functional dyspepsia, which lacks an identifiable structural origin. Differentiating dyspepsia from gallbladder disease is essential, as gallbladder disease often presents with right upper quadrant pain, especially after fatty meals, due to gallstones or cholecystitis.
Key Differences in Symptoms
Gallbladder disease primarily presents with intense pain in the upper right abdomen often radiating to the back or right shoulder, accompanied by nausea and vomiting, especially after fatty meals. Dyspepsia typically causes persistent discomfort or burning in the upper abdomen, bloating, early satiety, and occasional belching without severe localized pain. While gallbladder symptoms are usually acute and linked to fat ingestion, dyspepsia manifests as chronic, nonspecific digestive discomfort without clear relation to meal types.
Risk Factors Associated with Each Condition
Gallbladder disease risk factors include obesity, female gender, age over 40, rapid weight loss, and a family history of gallstones or gallbladder problems. Dyspepsia is often linked to Helicobacter pylori infection, chronic use of NSAIDs, smoking, stress, and dietary habits such as high-fat or spicy foods. Understanding these distinct risk factors aids in accurate diagnosis and targeted treatment for each gastrointestinal disorder.
Diagnostic Approaches: How Doctors Tell Them Apart
Gallbladder disease is primarily diagnosed through abdominal ultrasound, which detects gallstones, inflammation, or biliary obstruction, while dyspepsia diagnosis often involves upper endoscopy to identify gastritis, ulcers, or Barrett's esophagus. Laboratory tests such as liver function tests and pancreatic enzymes help differentiate gallbladder pathology from functional dyspepsia. Symptom assessment focusing on pain location, timing after meals, and associated nausea or jaundice further guides clinicians in distinguishing between these conditions.
Treatment Options for Gallbladder Disease
Treatment options for gallbladder disease primarily include cholecystectomy, which is the surgical removal of the gallbladder, often performed laparoscopically to reduce recovery time. Medication such as ursodeoxycholic acid can dissolve cholesterol gallstones but is generally less effective and reserved for patients who cannot undergo surgery. Pain management and dietary modifications focusing on low-fat intake help alleviate symptoms during acute episodes or as supportive care.
Management Strategies for Dyspepsia
Management strategies for dyspepsia prioritize lifestyle modifications such as dietary changes, stress reduction, and avoidance of irritants like alcohol and NSAIDs. Pharmacologic treatments commonly include proton pump inhibitors (PPIs), H2 receptor antagonists, and prokinetic agents to reduce acid production and improve gastric motility. When dyspepsia symptoms persist despite treatment, further evaluation with endoscopy is recommended to exclude gallbladder disease or other organic causes.
Complications: What Can Go Wrong?
Gallbladder disease can lead to serious complications such as cholecystitis, gallstones blocking the bile ducts, and pancreatitis, causing severe pain and infection risk. Dyspepsia primarily results in chronic indigestion, but if underlying conditions like peptic ulcers or gastroesophageal reflux disease (GERD) are present, it may cause bleeding, esophageal damage, or increased risk of gastric cancer. Early diagnosis and targeted treatment of these conditions are crucial to preventing life-threatening outcomes and long-term gastrointestinal damage.
Preventive Measures and Lifestyle Modifications
Effective preventive measures for gallbladder disease include maintaining a healthy weight, following a balanced diet rich in fiber and low in saturated fats, and regular physical activity to reduce the risk of gallstone formation. For dyspepsia, lifestyle modifications such as avoiding trigger foods like spicy or fatty meals, reducing alcohol intake, quitting smoking, and managing stress levels significantly help in minimizing symptoms. Both conditions benefit from meal portion control and avoiding late-night eating to promote optimal digestive health.
Gallbladder Disease Infographic
 libterm.com
libterm.com