Cholecystitis is the inflammation of the gallbladder, often caused by gallstones blocking the bile ducts, leading to severe abdominal pain and digestive issues. Prompt diagnosis and treatment are essential to prevent complications such as infection or gallbladder rupture. Discover how understanding symptoms and available treatments can protect your health by reading the full article.
Table of Comparison
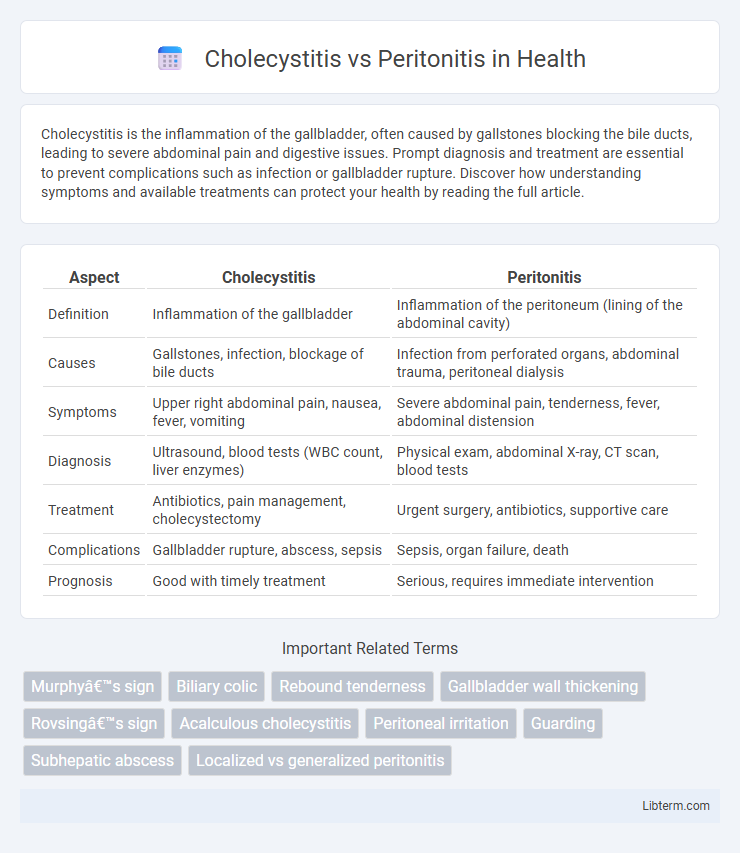
| Aspect | Cholecystitis | Peritonitis |
|---|---|---|
| Definition | Inflammation of the gallbladder | Inflammation of the peritoneum (lining of the abdominal cavity) |
| Causes | Gallstones, infection, blockage of bile ducts | Infection from perforated organs, abdominal trauma, peritoneal dialysis |
| Symptoms | Upper right abdominal pain, nausea, fever, vomiting | Severe abdominal pain, tenderness, fever, abdominal distension |
| Diagnosis | Ultrasound, blood tests (WBC count, liver enzymes) | Physical exam, abdominal X-ray, CT scan, blood tests |
| Treatment | Antibiotics, pain management, cholecystectomy | Urgent surgery, antibiotics, supportive care |
| Complications | Gallbladder rupture, abscess, sepsis | Sepsis, organ failure, death |
| Prognosis | Good with timely treatment | Serious, requires immediate intervention |
Introduction to Cholecystitis and Peritonitis
Cholecystitis is the inflammation of the gallbladder, primarily caused by gallstone obstruction leading to bile buildup, infection, and severe abdominal pain. Peritonitis is the inflammation of the peritoneum, the lining of the abdominal cavity, often resulting from infection due to perforation of abdominal organs or leakage of intestinal contents. Both conditions require prompt diagnosis and treatment to prevent serious complications such as sepsis or organ failure.
Definition: Cholecystitis Explained
Cholecystitis is the inflammation of the gallbladder, often caused by gallstones blocking the cystic duct, leading to severe abdominal pain and infection. Peritonitis refers to the inflammation of the peritoneum, the thin tissue lining the abdomen, typically resulting from infection or rupture of abdominal organs. Understanding the distinction is crucial, as cholecystitis is localized gallbladder inflammation, whereas peritonitis involves a widespread abdominal infection requiring urgent medical intervention.
Definition: Peritonitis Overview
Peritonitis is the inflammation of the peritoneum, the thin membrane lining the abdominal cavity and covering abdominal organs, usually caused by bacterial or fungal infection. It can result from conditions like a ruptured appendix, perforated ulcer, or abdominal injury, leading to severe abdominal pain, fever, and tenderness. Prompt diagnosis and treatment with antibiotics or surgery are critical to prevent complications such as sepsis and organ failure.
Etiology and Risk Factors
Cholecystitis primarily results from gallstone obstruction of the cystic duct, leading to inflammation and infection of the gallbladder, with risk factors including female gender, age over 40, obesity, and rapid weight loss. Peritonitis arises from bacterial or fungal infection due to perforation of abdominal organs, trauma, or postoperative complications, with risk factors such as abdominal surgery, gastrointestinal perforation, liver disease, and immunosuppression. Both conditions require prompt medical evaluation to prevent severe complications like sepsis and multi-organ failure.
Clinical Presentation: Signs and Symptoms
Cholecystitis typically presents with right upper quadrant abdominal pain, fever, nausea, and vomiting, often accompanied by a positive Murphy's sign indicating gallbladder inflammation. Peritonitis generally manifests as severe, diffuse abdominal pain, abdominal rigidity, rebound tenderness, and systemic signs like fever and tachycardia due to widespread peritoneal inflammation. Both conditions may cause abdominal tenderness, but the localized pain and Murphy's sign are key clinical features distinguishing cholecystitis from the generalized peritoneal signs of peritonitis.
Diagnostic Approaches and Imaging
Diagnostic approaches for cholecystitis primarily involve abdominal ultrasound, which detects gallbladder wall thickening, stones, and pericholecystic fluid, while hepatobiliary iminodiacetic acid (HIDA) scans assess cystic duct obstruction. Peritonitis diagnosis relies on clinical evaluation, peritoneal fluid analysis, and imaging modalities like abdominal X-rays and computed tomography (CT) scans to identify free intraperitoneal air or fluid indicative of inflammation or infection. CT imaging provides comprehensive visualization in peritonitis, differentiating localized abscesses from widespread peritoneal involvement, whereas ultrasound remains the first-line tool for cholecystitis identification.
Laboratory Findings Comparison
Cholecystitis typically presents with elevated white blood cell count (leukocytosis) and mildly increased liver enzymes such as alanine aminotransferase (ALT) and alkaline phosphatase (ALP), with normal or slightly elevated bilirubin levels. In peritonitis, laboratory findings show marked leukocytosis, elevated inflammatory markers like C-reactive protein (CRP) and procalcitonin, along with metabolic acidosis and electrolyte imbalances due to systemic inflammatory response. Blood cultures may be positive in peritonitis indicating sepsis, whereas cholecystitis often reveals localized infection with positive bile cultures in some cases.
Complications and Prognosis
Cholecystitis, an inflammation of the gallbladder often caused by gallstones, can lead to complications such as gallbladder rupture, abscess formation, and sepsis if untreated. Peritonitis, the inflammation of the peritoneum usually due to infection or perforation of abdominal organs, carries a higher risk of severe systemic infection, septic shock, and multi-organ failure. The prognosis of cholecystitis generally improves with timely cholecystectomy and antibiotics, whereas peritonitis requires urgent surgical intervention and intensive care, with prognosis highly dependent on the rapidity of diagnosis and treatment.
Treatment and Management Strategies
Cholecystitis treatment primarily involves antibiotics to target infection, pain management, and often laparoscopic cholecystectomy for definitive removal of the inflamed gallbladder. Peritonitis requires urgent surgical intervention to eliminate the source of infection combined with broad-spectrum intravenous antibiotics and intensive supportive care, including fluid resuscitation and organ function monitoring. Early diagnosis and targeted therapy significantly improve outcomes in both conditions, with postoperative care focusing on preventing complications like sepsis or abscess formation.
Prevention and Patient Education
Preventing cholecystitis involves maintaining a healthy diet low in fatty foods and managing risk factors such as obesity and gallstones through regular medical check-ups. Patient education should emphasize recognizing early symptoms like abdominal pain and seeking prompt medical attention to avoid complications. For peritonitis prevention, sterile surgical techniques and timely treatment of abdominal infections are critical, alongside educating patients on signs of infection such as fever and severe abdominal tenderness to ensure early diagnosis and intervention.
Cholecystitis Infographic
 libterm.com
libterm.com