Necrosis is the irreversible death of cells or tissue caused by factors such as infection, toxins, or trauma, leading to the breakdown and dysfunction of affected areas. This process often results in inflammation and can significantly impair your body's ability to heal, sometimes requiring medical intervention to prevent further damage. Explore the rest of this article to understand the causes, symptoms, and treatments associated with necrosis.
Table of Comparison
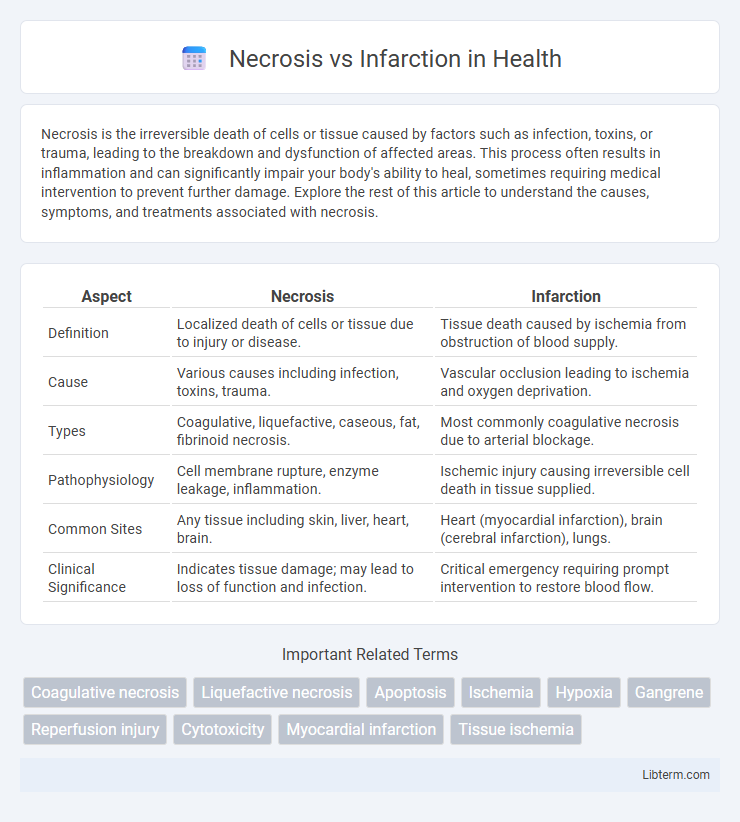
| Aspect | Necrosis | Infarction |
|---|---|---|
| Definition | Localized death of cells or tissue due to injury or disease. | Tissue death caused by ischemia from obstruction of blood supply. |
| Cause | Various causes including infection, toxins, trauma. | Vascular occlusion leading to ischemia and oxygen deprivation. |
| Types | Coagulative, liquefactive, caseous, fat, fibrinoid necrosis. | Most commonly coagulative necrosis due to arterial blockage. |
| Pathophysiology | Cell membrane rupture, enzyme leakage, inflammation. | Ischemic injury causing irreversible cell death in tissue supplied. |
| Common Sites | Any tissue including skin, liver, heart, brain. | Heart (myocardial infarction), brain (cerebral infarction), lungs. |
| Clinical Significance | Indicates tissue damage; may lead to loss of function and infection. | Critical emergency requiring prompt intervention to restore blood flow. |
Understanding Necrosis: Definition and Causes
Necrosis refers to the premature death of cells or tissues caused by factors such as infection, toxins, trauma, or ischemia. It involves unregulated cell death resulting in inflammation and damage to surrounding tissues. Common causes include exposure to harmful agents, physical injury, or lack of blood supply leading to cellular disruption and membrane breakdown.
What Is Infarction? Key Concepts Explained
Infarction refers to tissue death caused by an inadequate blood supply, resulting in oxygen deprivation and cellular damage. It often occurs due to the obstruction of arterial blood flow, commonly seen in conditions like myocardial infarction and cerebral infarction. Unlike general necrosis, infarction specifically involves ischemic injury leading to localized tissue death.
Pathophysiological Differences: Necrosis vs Infarction
Necrosis is the uncontrolled death of cells caused by external factors such as infection, toxins, or trauma, resulting in the breakdown of cell membranes and release of intracellular contents. Infarction is a specific type of necrosis caused by ischemia leading to tissue death due to the sudden loss of blood supply, primarily affecting organs like the heart, brain, and kidneys. The key pathophysiological difference lies in infarction being ischemic necrosis with defined vascular occlusion, whereas necrosis encompasses a broader range of cell death mechanisms without necessarily involving ischemia.
Types of Necrosis: Classification and Examples
Necrosis is classified into several types based on tissue characteristics and causative factors, including coagulative necrosis commonly seen in myocardial infarction, liquefactive necrosis typically found in brain abscesses, caseous necrosis associated with tuberculosis, fat necrosis resulting from pancreatic enzyme activity, and fibrinoid necrosis linked to immune reactions in blood vessels. Each type exhibits distinct histopathological features such as coagulation of proteins in coagulative necrosis or enzyme-mediated tissue digestion in liquefactive necrosis, which aids in differential diagnosis. Understanding these classifications is crucial for identifying the underlying pathology and guiding appropriate clinical treatment strategies.
Types of Infarction: Classification and Examples
Types of infarction are classified based on the affected tissue and the presence of oxygen delivery, with the main categories being red (hemorrhagic) and white (anemic) infarctions. Red infarctions typically occur in organs with dual blood supplies such as the lungs and intestines, where reperfusion leads to hemorrhage into the necrotic area. White infarctions are common in solid organs like the heart, kidney, and spleen, where arterial occlusion leads to pale, coagulative necrosis due to lack of collateral circulation.
Cellular Mechanisms: How Necrosis and Infarction Occur
Necrosis involves uncontrolled cell death due to factors like toxins, infections, or trauma, leading to cell membrane rupture and inflammation. Infarction occurs when ischemia causes prolonged oxygen deprivation, resulting in localized tissue death primarily through coagulative necrosis. Both processes trigger distinct cellular mechanisms, with necrosis involving enzymatic digestion of cell components and infarction characterized by irreversible hypoxic injury and loss of ATP production.
Clinical Manifestations: Signs and Symptoms Compared
Necrosis presents with localized pain, swelling, and tissue discoloration, often accompanied by loss of function in the affected area, while infarction typically causes sudden, severe pain and possible organ dysfunction due to ischemia. Infarction's clinical signs include pallor, cyanosis, and later, tissue necrosis, reflecting irreversible cellular death, whereas necrosis itself manifests as softening, liquefaction, or gangrene formation depending on the underlying cause. Systemic symptoms such as fever, increased white blood cell count, and malaise can occur in both conditions, indicating an inflammatory response to tissue injury.
Diagnostic Approaches: Differentiating Necrosis and Infarction
Histopathological examination remains the gold standard for differentiating necrosis from infarction, with necrosis showing localized cell death due to injury and infarction characterized by tissue death caused by ischemia. Imaging techniques like MRI and CT scans assist in identifying infarcted regions, especially in organs such as the brain, heart, and lungs, by highlighting areas of reduced blood flow and tissue damage. Biomarkers including elevated lactate dehydrogenase (LDH) and creatine kinase (CK) levels support the diagnosis by indicating cellular injury and ischemic processes.
Treatment Strategies: Managing Necrosis and Infarction
Treatment strategies for necrosis focus on removing dead tissue through debridement and preventing infection with antibiotics and wound care, while infarction management emphasizes restoring blood flow using thrombolytics, anticoagulants, or surgical intervention. Hyperbaric oxygen therapy may enhance healing in necrotic tissue by improving oxygenation, whereas infarction treatment includes addressing underlying causes such as atherosclerosis or embolism to prevent recurrence. Supportive measures like pain control and monitoring organ function are critical in both necrosis and infarction management to optimize recovery and minimize complications.
Prognosis and Complications: Long-term Outcomes
Necrosis often leads to tissue degradation with variable prognosis depending on the cause and extent of damage, while infarction, characterized by ischemic cell death, typically results in more localized and predictable tissue injury, often complicating with scar formation or organ dysfunction. Long-term outcomes of infarction include potential heart failure, arrhythmias, or chronic ischemic conditions, whereas necrosis may result in persistent inflammation or secondary infections. Both conditions require careful monitoring to prevent complications such as sepsis in necrosis or chronic ischemic damage in infarction.
Necrosis Infographic
 libterm.com
libterm.com