Hypophosphatemia is a condition characterized by abnormally low levels of phosphate in the blood, which can lead to muscle weakness, bone pain, and respiratory issues. Early diagnosis and treatment are crucial to prevent severe complications and restore normal phosphate balance. Explore the full article to understand the causes, symptoms, and effective management strategies for hypophosphatemia.
Table of Comparison
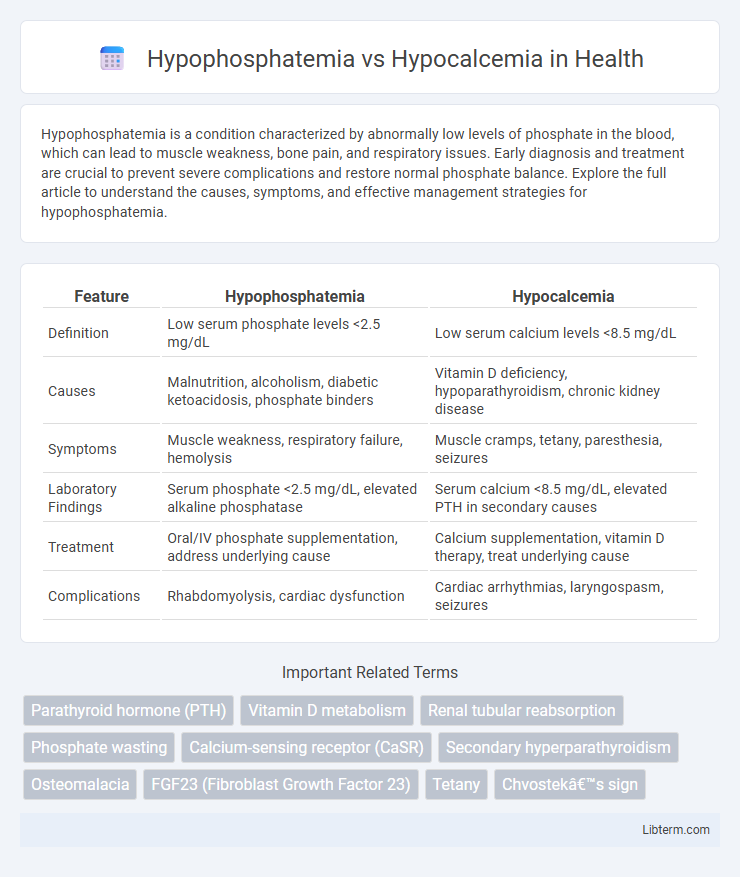
| Feature | Hypophosphatemia | Hypocalcemia |
|---|---|---|
| Definition | Low serum phosphate levels <2.5 mg/dL | Low serum calcium levels <8.5 mg/dL |
| Causes | Malnutrition, alcoholism, diabetic ketoacidosis, phosphate binders | Vitamin D deficiency, hypoparathyroidism, chronic kidney disease |
| Symptoms | Muscle weakness, respiratory failure, hemolysis | Muscle cramps, tetany, paresthesia, seizures |
| Laboratory Findings | Serum phosphate <2.5 mg/dL, elevated alkaline phosphatase | Serum calcium <8.5 mg/dL, elevated PTH in secondary causes |
| Treatment | Oral/IV phosphate supplementation, address underlying cause | Calcium supplementation, vitamin D therapy, treat underlying cause |
| Complications | Rhabdomyolysis, cardiac dysfunction | Cardiac arrhythmias, laryngospasm, seizures |
Understanding Hypophosphatemia and Hypocalcemia
Hypophosphatemia is characterized by abnormally low serum phosphate levels below 2.5 mg/dL, often leading to muscle weakness, respiratory failure, and impaired cellular function due to disrupted ATP production. Hypocalcemia involves reduced serum calcium levels under 8.5 mg/dL, manifesting as neuromuscular irritability, tetany, and cardiac arrhythmias resulting from altered membrane excitability. Both conditions require precise biochemical evaluation and targeted management to restore mineral balance and prevent critical complications.
Causes of Hypophosphatemia
Hypophosphatemia primarily results from inadequate dietary intake, increased renal phosphate excretion, or intracellular phosphate shifts due to conditions such as refeeding syndrome or respiratory alkalosis. It is commonly seen in patients with chronic alcoholism, malnutrition, or those receiving parenteral nutrition without adequate phosphate supplementation. Unlike hypocalcemia, which is often caused by vitamin D deficiency or hypoparathyroidism, hypophosphatemia is strongly linked to disorders affecting phosphate metabolism and renal tubular function.
Causes of Hypocalcemia
Hypocalcemia is primarily caused by vitamin D deficiency, hypoparathyroidism, chronic kidney disease, and magnesium deficiency, which impair calcium absorption or regulation. In contrast, hypophosphatemia commonly results from malnutrition, refeeding syndrome, or shifts of phosphate into cells during alkalosis or cellular uptake. Hypocalcemia's disruption of neuromuscular function and cardiovascular stability distinguishes its clinical urgency from the metabolic disturbances seen in hypophosphatemia.
Pathophysiology: How Each Condition Develops
Hypophosphatemia develops due to decreased intestinal absorption, increased renal excretion, or intracellular shifts of phosphate, often linked to vitamin D deficiency, malnutrition, or hyperparathyroidism. Hypocalcemia results from impaired calcium absorption, excessive calcium losses, or disrupted parathyroid hormone (PTH) function, commonly caused by hypoparathyroidism, vitamin D deficiency, or chronic kidney disease. Both conditions involve disturbances in mineral metabolism but affect different regulatory pathways and organs, with phosphate primarily influenced by renal handling and calcium tightly controlled by PTH and vitamin D interactions.
Common Signs and Symptoms
Hypophosphatemia commonly presents with muscle weakness, irritability, and confusion due to low phosphate levels affecting cellular energy metabolism. Hypocalcemia is characterized by tetany, paresthesia, and positive Chvostek or Trousseau signs linked to decreased calcium concentrations impacting neuromuscular excitability. Both conditions may cause seizures and cardiac arrhythmias, reflecting electrolyte imbalance consequences on nervous and muscular systems.
Diagnostic Approaches: Differentiating the Disorders
Diagnostic approaches for hypophosphatemia and hypocalcemia center on precise serum measurements of phosphate and calcium levels, respectively, combined with assessment of parathyroid hormone (PTH) and vitamin D metabolites to identify underlying metabolic disturbances. Hypophosphatemia is often distinguished by low serum phosphate with normal or elevated calcium, necessitating evaluation of renal phosphate wasting through fractional excretion tests, while hypocalcemia features low serum calcium accompanied by altered PTH response, highlighting disorders such as hypoparathyroidism or vitamin D deficiency. Advanced imaging and genetic testing may be employed to differentiate inherited disorders affecting phosphate or calcium metabolism, ensuring targeted therapeutic strategies.
Laboratory Findings and Interpretation
Hypophosphatemia is characterized by serum phosphate levels below 2.5 mg/dL, often accompanied by normal or elevated serum calcium and decreased urinary phosphate excretion, indicating impaired phosphate absorption or shifting into cells. In contrast, hypocalcemia presents with serum calcium levels less than 8.5 mg/dL, frequently associated with elevated serum phosphate, reduced parathyroid hormone (PTH) levels, and increased urinary calcium excretion, reflecting disturbances in calcium metabolism. Interpretation of these laboratory findings requires evaluation of serum electrolytes, PTH levels, vitamin D status, and renal function to differentiate underlying causes and guide targeted management.
Treatment Strategies for Hypophosphatemia vs Hypocalcemia
Treatment strategies for hypophosphatemia typically involve oral or intravenous phosphate replacement to restore serum phosphate levels, with careful monitoring to avoid complications such as hypocalcemia or hyperphosphatemia. In contrast, hypocalcemia treatment prioritizes calcium supplementation, either orally or intravenously, alongside addressing underlying causes like vitamin D deficiency or hypoparathyroidism to normalize serum calcium levels. Both conditions require electrolyte balance monitoring and correction of associated abnormalities to prevent neuromuscular and cardiac complications.
Complications and Long-Term Outcomes
Hypophosphatemia can lead to complications such as muscle weakness, respiratory failure, and impaired cardiac function, with long-term outcomes including bone demineralization and osteomalacia. Hypocalcemia often results in neuromuscular irritability, tetany, seizures, and cardiac arrhythmias, with chronic deficiency causing osteoporosis and calcification of basal ganglia. Both conditions require careful monitoring to prevent irreversible damage, but hypophosphatemia predominantly affects energy metabolism while hypocalcemia mainly disrupts neuromuscular and cardiovascular systems.
Preventive Measures and Patient Education
Preventive measures for hypophosphatemia include maintaining adequate dietary phosphate intake and monitoring phosphate levels in patients with risk factors such as malnutrition or chronic alcohol use, while hypocalcemia prevention focuses on ensuring sufficient calcium and vitamin D consumption and regular screening in high-risk groups like those with kidney disease or hypoparathyroidism. Patient education should emphasize recognizing early symptoms such as muscle weakness for hypophosphatemia and numbness or tingling for hypocalcemia, adherence to prescribed supplements, and prompt medical follow-up to avoid complications including bone density loss or cardiac arrhythmias. Both conditions require personalized guidance on nutrition, medication management, and routine laboratory evaluations to effectively prevent recurrence.
Hypophosphatemia Infographic
 libterm.com
libterm.com