Tendonitis is the inflammation of a tendon, often causing pain and restricted movement near joints such as the shoulder, elbow, or knee. It frequently results from repetitive motions or overuse, making it common in athletes and individuals with physically demanding jobs. Discover effective treatments and prevention tips to protect your tendons by reading the full article.
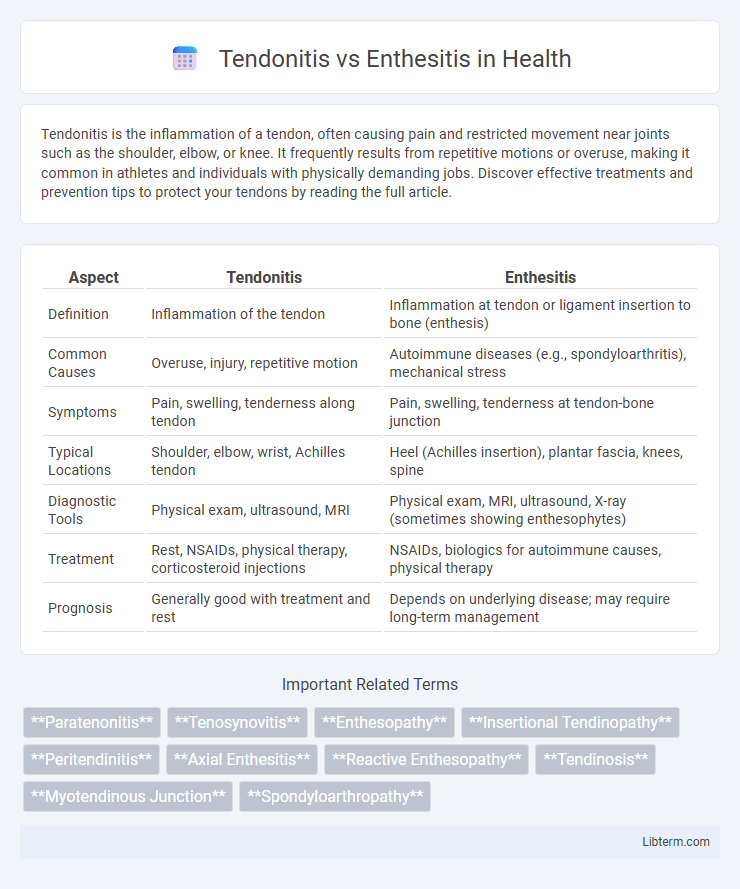
Table of Comparison
| Aspect | Tendonitis | Enthesitis |
|---|---|---|
| Definition | Inflammation of the tendon | Inflammation at tendon or ligament insertion to bone (enthesis) |
| Common Causes | Overuse, injury, repetitive motion | Autoimmune diseases (e.g., spondyloarthritis), mechanical stress |
| Symptoms | Pain, swelling, tenderness along tendon | Pain, swelling, tenderness at tendon-bone junction |
| Typical Locations | Shoulder, elbow, wrist, Achilles tendon | Heel (Achilles insertion), plantar fascia, knees, spine |
| Diagnostic Tools | Physical exam, ultrasound, MRI | Physical exam, MRI, ultrasound, X-ray (sometimes showing enthesophytes) |
| Treatment | Rest, NSAIDs, physical therapy, corticosteroid injections | NSAIDs, biologics for autoimmune causes, physical therapy |
| Prognosis | Generally good with treatment and rest | Depends on underlying disease; may require long-term management |
Understanding Tendonitis: Definition and Causes
Tendonitis is the inflammation or irritation of a tendon, the thick fibrous cords that attach muscle to bone, commonly caused by repetitive motion or acute injury. Factors such as overuse, improper technique, and underlying conditions like arthritis contribute to the development of tendonitis. Understanding the mechanical stress and microtears involved is essential for effective treatment and prevention.
What is Enthesitis? Key Characteristics
Enthesitis is the inflammation of entheses, the sites where tendons or ligaments attach to bone, often linked to autoimmune diseases like psoriatic arthritis or ankylosing spondylitis. Key characteristics of enthesitis include localized pain, tenderness, and swelling at these attachment points, commonly affecting areas such as the Achilles tendon, plantar fascia, and lateral epicondyle. Unlike tendonitis, which is inflammation of the tendon itself, enthesitis specifically targets the bone-tendon junction, causing distinct symptoms and requiring specialized diagnostic approaches.
Anatomical Differences: Tendonitis vs Enthesitis
Tendonitis involves inflammation of the tendon itself, typically occurring along the length of the tendon where it connects muscle to bone. Enthesitis specifically affects the enthesis, the critical anatomical site where tendons or ligaments attach directly to the bone, often leading to localized pain and swelling. These differences highlight that tendonitis is primarily a tendon pathology, whereas enthesitis represents inflammation at the tendon-bone junction.
Common Symptoms: Comparing Clinical Presentations
Tendonitis typically presents with localized pain, swelling, and tenderness at the tendon site, often worsening with movement or pressure. Enthesitis involves inflammation at the enthesis, the tendon or ligament attachment to bone, causing deep, aching pain and stiffness, particularly common in conditions like spondyloarthritis. Both conditions may show overlapping symptoms, but enthesitis often includes bone tenderness and morning stiffness, while tendonitis pain is more activity-specific and acute.
Underlying Risk Factors and Associated Conditions
Tendonitis primarily results from repetitive strain or overuse, often occurring in athletes or individuals with occupations requiring repetitive motions, while enthesitis is strongly linked to autoimmune conditions like spondyloarthritis and psoriatic arthritis. Underlying risk factors for tendonitis include aging, poor biomechanics, and sudden increases in activity, whereas enthesitis is frequently associated with genetic predispositions such as HLA-B27 positivity. Both conditions may present with localized pain and inflammation, but enthesitis also involves inflammation at the tendon or ligament attachment to bone, reflecting its connection to systemic inflammatory diseases.
Diagnostic Techniques: How to Distinguish the Two
Diagnostic techniques for distinguishing tendonitis from enthesitis include ultrasound and MRI, which provide detailed images of soft tissues, highlighting inflammation patterns at the tendon itself in tendonitis versus inflammation at tendon-to-bone insertion sites characteristic of enthesitis. Clinical examination focuses on localized pain and swelling, with enthesitis often presenting tenderness directly over bony prominences, whereas tendonitis pain is more diffuse along the tendon shaft. Laboratory tests, including inflammatory markers and autoimmune panels, assist in diagnosing enthesitis associated with spondyloarthropathies, differentiating it from isolated tendonitis caused by mechanical overuse.
Treatment Approaches for Tendonitis
Tendonitis treatment primarily involves rest, ice application, and nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation in the affected tendon. Physical therapy focusing on stretching and strengthening exercises helps restore tendon function and prevent recurrence. In severe or chronic cases, corticosteroid injections or platelet-rich plasma (PRP) therapy may be considered to enhance healing and reduce symptoms.
Management Strategies for Enthesitis
Management strategies for enthesitis primarily include targeted anti-inflammatory treatments such as nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroid injections to reduce pain and inflammation at the tendon or ligament insertion sites. Physical therapy focusing on stretching and strengthening exercises improves flexibility and supports proper joint function, while biologic agents like tumor necrosis factor (TNF) inhibitors are effective in severe or refractory cases, especially when associated with spondyloarthropathies. Monitoring disease progression with imaging techniques such as ultrasound or MRI aids in tailoring treatment plans and preventing further enthesal damage.
Prevention Tips for Both Conditions
Preventing tendonitis and enthesitis involves maintaining proper joint alignment during physical activities, using appropriate warm-up and stretching techniques, and avoiding repetitive strain by alternating tasks or incorporating rest periods. Strengthening surrounding muscles through targeted exercises enhances joint stability, reducing inflammation risks at tendon and enthesis sites. Monitoring early signs such as localized pain or stiffness and seeking prompt medical advice supports early intervention and minimizes chronic complications.
When to Seek Medical Advice: Red Flags and Next Steps
Persistent joint pain accompanied by swelling, redness, or warmth may indicate tendonitis or enthesitis requiring immediate medical evaluation. Inability to move the affected area, severe pain unresponsive to over-the-counter medications, or systemic symptoms like fever are red flags signaling the need for specialist consultation. Early diagnosis through imaging techniques such as ultrasound or MRI improves treatment outcomes and prevents chronic complications.
Tendonitis Infographic
 libterm.com
libterm.com