Night blindness impairs your ability to see clearly in low-light conditions, often caused by vitamin A deficiency or underlying eye disorders like retinitis pigmentosa. Early diagnosis and treatment are crucial to prevent worsening vision and improve nighttime visibility. Explore the rest of the article to learn more about symptoms, causes, and effective management strategies for night blindness.
Table of Comparison
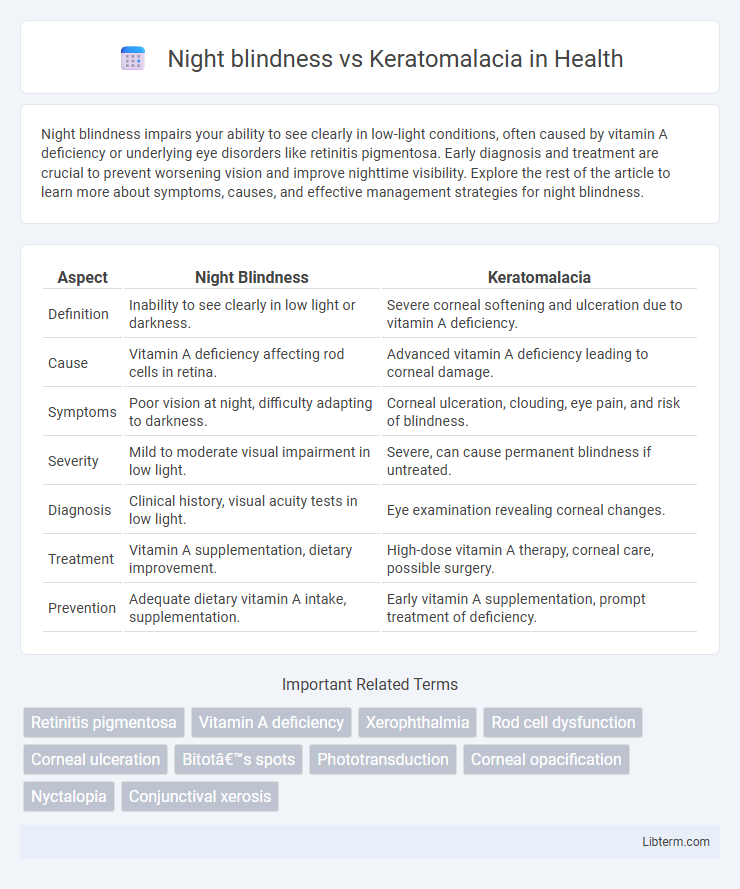
| Aspect | Night Blindness | Keratomalacia |
|---|---|---|
| Definition | Inability to see clearly in low light or darkness. | Severe corneal softening and ulceration due to vitamin A deficiency. |
| Cause | Vitamin A deficiency affecting rod cells in retina. | Advanced vitamin A deficiency leading to corneal damage. |
| Symptoms | Poor vision at night, difficulty adapting to darkness. | Corneal ulceration, clouding, eye pain, and risk of blindness. |
| Severity | Mild to moderate visual impairment in low light. | Severe, can cause permanent blindness if untreated. |
| Diagnosis | Clinical history, visual acuity tests in low light. | Eye examination revealing corneal changes. |
| Treatment | Vitamin A supplementation, dietary improvement. | High-dose vitamin A therapy, corneal care, possible surgery. |
| Prevention | Adequate dietary vitamin A intake, supplementation. | Early vitamin A supplementation, prompt treatment of deficiency. |
Introduction to Night Blindness and Keratomalacia
Night blindness, medically known as nyctalopia, refers to the impaired ability to see in low light or darkness, often caused by vitamin A deficiency or retinal disorders. Keratomalacia is a severe, progressive eye condition characterized by the softening and ulceration of the cornea due to advanced vitamin A deficiency, leading to potential blindness. Both conditions are interconnected through vitamin A deficiency but affect different parts of the eye, with night blindness impacting retinal function and keratomalacia damaging the corneal structure.
Understanding Night Blindness: Definition and Causes
Night blindness, or nyctalopia, is a visual impairment characterized by difficulty seeing in low light or darkness, often caused by vitamin A deficiency, retinitis pigmentosa, or cataracts. Keratomalacia is a severe eye disorder resulting from prolonged vitamin A deficiency, leading to corneal softening, ulceration, and potential blindness. Understanding night blindness requires recognizing its primary causes, especially vitamin A deficiency, which also underpins the development of keratomalacia in advanced cases.
What is Keratomalacia?
Keratomalacia is a severe eye disorder caused by vitamin A deficiency, leading to the softening and ulceration of the cornea. Unlike night blindness, which primarily impairs vision in low-light conditions due to early vitamin A deficiency, keratomalacia represents an advanced stage, often resulting in permanent corneal damage and potential blindness. Prompt treatment with vitamin A supplementation is critical to prevent irreversible vision loss and complications associated with keratomalacia.
Role of Vitamin A in Eye Health
Vitamin A plays a crucial role in maintaining eye health by supporting the production of rhodopsin, a pigment critical for low-light vision, preventing conditions like night blindness. Night blindness results from insufficient vitamin A, impairing retinal function and dark adaptation. Keratomalacia, a severe consequence of prolonged vitamin A deficiency, leads to corneal softening and potential blindness, highlighting the vitamin's essential role in corneal integrity and repair.
Comparing Symptoms: Night Blindness vs Keratomalacia
Night blindness primarily manifests as difficulty seeing in low light or darkness, often caused by vitamin A deficiency, retinitis pigmentosa, or cataracts. Keratomalacia, a severe consequence of prolonged vitamin A deficiency, presents with symptoms including corneal clouding, ulceration, and softening, leading to significant vision loss and potential blindness. While night blindness affects vision in dim environments, keratomalacia results in structural eye damage and more profound, often irreversible vision impairment.
Risk Factors for Night Blindness and Keratomalacia
Night blindness primarily results from vitamin A deficiency, malnutrition, or underlying retinal disorders, increasing the risk in populations with inadequate dietary intake of vitamin A and those suffering from chronic illnesses affecting nutrient absorption. Keratomalacia, a severe manifestation of vitamin A deficiency, occurs predominantly in children and individuals with prolonged malnutrition or malabsorption syndromes, leading to corneal softening and potential blindness. Populations in developing countries with limited access to nutrient-rich foods are at heightened risk for both conditions due to persistent vitamin A deficiency and poor overall health status.
Diagnostic Approaches for Both Conditions
Night blindness diagnosis primarily involves a thorough patient history, assessment of visual function under low-light conditions, and electroretinography to evaluate rod photoreceptor activity. Keratomalacia diagnosis requires clinical examination revealing corneal softness and ulceration, supported by biochemical tests such as serum retinol levels indicating severe vitamin A deficiency. Imaging techniques and slit-lamp microscopy are essential for assessing corneal integrity and differentiating keratomalacia from other corneal pathologies.
Treatment Options: Night Blindness vs Keratomalacia
Treatment options for night blindness primarily involve vitamin A supplementation to address underlying deficiencies, improving retinal function and vision in low-light conditions. Keratomalacia requires urgent high-dose vitamin A therapy combined with supportive care to prevent corneal ulceration and potential blindness, often necessitating hospitalization. Both conditions also benefit from dietary improvements rich in vitamin A to ensure long-term ocular health and prevent recurrence.
Prevention Strategies for Eye Disorders
Night blindness prevention focuses on maintaining adequate vitamin A levels through a diet rich in carrots, leafy greens, and fortified foods, as vitamin A deficiency is the primary cause. Keratomalacia prevention requires early intervention with high-dose vitamin A supplementation and addressing underlying malnutrition to prevent corneal softening and blindness. Regular eye screenings and education on vitamin A sources are critical strategies to reduce the incidence of these vitamin A deficiency-related eye disorders.
Prognosis and Long-Term Management
Night blindness primarily results from vitamin A deficiency and typically shows improvement with prompt vitamin A supplementation, offering a favorable prognosis when addressed early. Keratomalacia, a severe manifestation of vitamin A deficiency, leads to corneal softening and ulceration, often causing permanent vision loss without aggressive treatment. Long-term management for both conditions involves sustained vitamin A intake, regular ophthalmologic monitoring, and addressing underlying nutritional deficiencies to prevent recurrence and complications.
Night blindness Infographic
 libterm.com
libterm.com