Leukoplakia is a condition characterized by white patches on the tongue or inside the mouth, often caused by chronic irritation, smoking, or other factors, and may carry a risk of progressing to oral cancer. Oral candidiasis, also known as thrush, is a fungal infection caused by Candida species that results in white, creamy lesions and discomfort in the oral cavity, particularly in immunocompromised individuals or those using inhaled steroids. Discover how these oral conditions differ in symptoms, causes, and treatment options to protect Your oral health effectively.
Table of Comparison
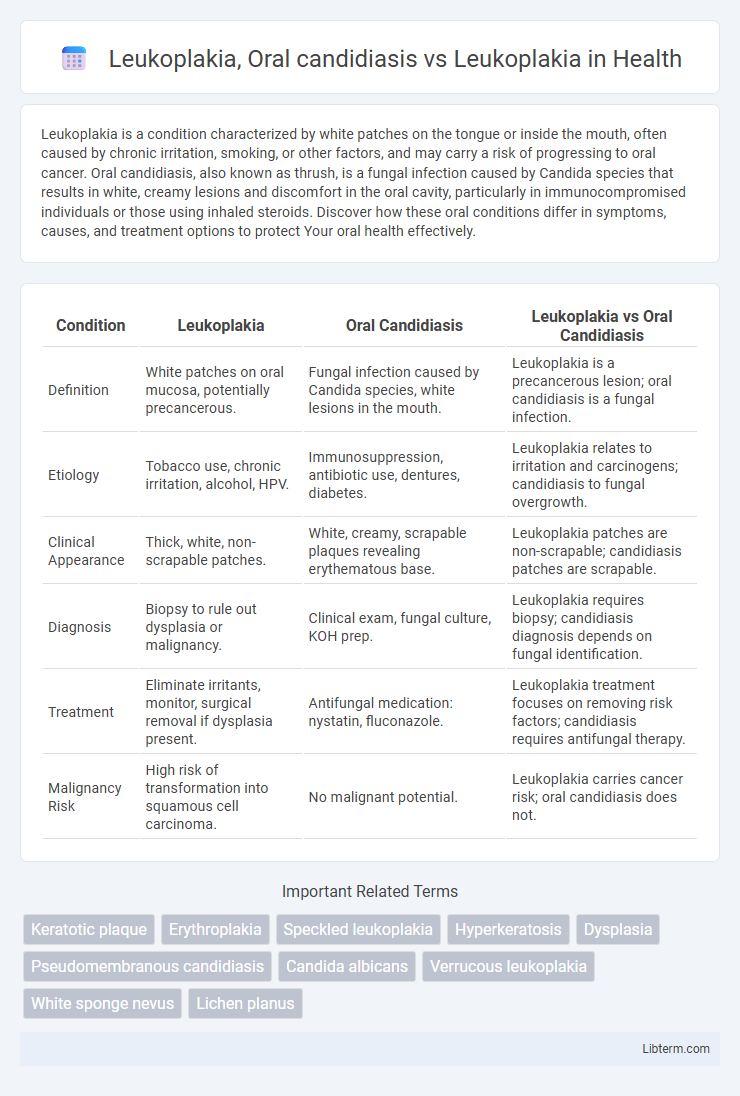
| Condition | Leukoplakia | Oral Candidiasis | Leukoplakia vs Oral Candidiasis |
|---|---|---|---|
| Definition | White patches on oral mucosa, potentially precancerous. | Fungal infection caused by Candida species, white lesions in the mouth. | Leukoplakia is a precancerous lesion; oral candidiasis is a fungal infection. |
| Etiology | Tobacco use, chronic irritation, alcohol, HPV. | Immunosuppression, antibiotic use, dentures, diabetes. | Leukoplakia relates to irritation and carcinogens; candidiasis to fungal overgrowth. |
| Clinical Appearance | Thick, white, non-scrapable patches. | White, creamy, scrapable plaques revealing erythematous base. | Leukoplakia patches are non-scrapable; candidiasis patches are scrapable. |
| Diagnosis | Biopsy to rule out dysplasia or malignancy. | Clinical exam, fungal culture, KOH prep. | Leukoplakia requires biopsy; candidiasis diagnosis depends on fungal identification. |
| Treatment | Eliminate irritants, monitor, surgical removal if dysplasia present. | Antifungal medication: nystatin, fluconazole. | Leukoplakia treatment focuses on removing risk factors; candidiasis requires antifungal therapy. |
| Malignancy Risk | High risk of transformation into squamous cell carcinoma. | No malignant potential. | Leukoplakia carries cancer risk; oral candidiasis does not. |
Understanding Leukoplakia: Definition and Causes
Leukoplakia is characterized by thickened, white patches on the mucous membranes of the oral cavity, primarily caused by chronic irritation from tobacco use, alcohol consumption, or rough teeth surfaces. Unlike oral candidiasis, which results from a fungal infection by Candida species presenting as white, removable plaques often associated with immunosuppression or antibiotic use, leukoplakia lesions are non-removable and considered potentially precancerous. Understanding leukoplakia's etiology involves identifying risk factors such as tobacco exposure and mechanical irritation, which lead to epithelial hyperplasia and possible dysplasia, necessitating clinical monitoring and biopsy for malignant transformation assessment.
Oral Candidiasis vs Leukoplakia: Key Differences
Oral candidiasis is a fungal infection caused by Candida species, presenting as white, curd-like patches that can be scraped off, often accompanied by redness or soreness. Leukoplakia, in contrast, manifests as persistent, non-scrapable white plaques on the oral mucosa, potentially representing precancerous lesions. The key differences lie in etiology--fungal infection versus abnormal epithelial growth--and clinical presentation, which guides diagnosis and management strategies.
Risk Factors for Leukoplakia and Oral Candidiasis
Leukoplakia primarily develops due to chronic irritation from tobacco use, alcohol consumption, and human papillomavirus (HPV) infection, with risk factors including age, immune suppression, and poor oral hygiene. Oral candidiasis risk factors consist of immunosuppressive conditions like HIV/AIDS, diabetes mellitus, prolonged antibiotic or corticosteroid use, and denture wear, which promotes fungal overgrowth. Both conditions share immunocompromised states as significant overlapping risk factors, yet leukoplakia is more closely linked to carcinogenic exposures while oral candidiasis is rooted in fungal colonization and imbalance.
Clinical Presentation: Recognizing Lesions
Leukoplakia presents as white or grayish patches on the oral mucosa that cannot be scraped off and are often asymptomatic, posing a risk of malignant transformation. Oral candidiasis, in contrast, shows white, creamy plaques that can be easily wiped away, revealing erythematous and sometimes bleeding mucosa underneath. Recognizing the persistence and texture of lesions helps differentiate leukoplakia's non-removable plaques from the removable pseudomembranous patches characteristic of oral candidiasis.
Diagnostic Approaches for Oral White Lesions
Leukoplakia and oral candidiasis are primary causes of oral white lesions requiring distinct diagnostic approaches. Leukoplakia diagnosis relies on clinical examination combined with biopsy to rule out dysplasia or malignancy, while oral candidiasis diagnosis involves clinical evaluation supported by microbiological cultures or cytology to detect Candida species. Accurate differentiation is essential to guide appropriate treatment and management strategies.
Histopathological Features: Leukoplakia vs Candidiasis
Leukoplakia histopathology reveals hyperkeratosis, acanthosis, and potential epithelial dysplasia characterized by cellular atypia and increased mitotic figures, posing a risk for malignant transformation. Oral candidiasis typically presents with epithelial hyperplasia, neutrophilic microabscesses, and presence of pseudohyphae or yeast forms invading the superficial epithelium, confirmed by PAS or silver staining. The distinction lies in leukoplakia's premalignant epithelial changes versus candidiasis' fungal-induced inflammatory response with fungal elements within the mucosa.
Treatment Strategies for Leukoplakia and Oral Candidiasis
Treatment strategies for leukoplakia primarily involve eliminating potential irritants such as tobacco and alcohol, regular monitoring for malignant transformation, and surgical excision or laser therapy for lesions with dysplasia. Oral candidiasis treatment focuses on antifungal agents like nystatin, fluconazole, or clotrimazole to eradicate Candida albicans infection. Distinguishing between leukoplakia and oral candidiasis is critical as their management diverges: leukoplakia requires vigilant follow-up due to its premalignant potential, whereas oral candidiasis typically resolves with targeted antifungal therapy.
Malignant Transformation Risk: Leukoplakia
Leukoplakia carries a significant malignant transformation risk, with studies estimating a progression rate of 1-20% depending on histopathological features such as dysplasia severity. Oral candidiasis, typically a fungal infection caused by Candida species, rarely undergoes malignant transformation and is generally considered a benign condition. Persistent leukoplakia lesions with epithelial dysplasia require close monitoring and biopsy to manage the potential progression to oral squamous cell carcinoma.
Prevention and Oral Health Management
Leukoplakia prevention centers on avoiding tobacco and alcohol, maintaining rigorous oral hygiene, and having regular dental check-ups to monitor any white patches in the mouth. Oral candidiasis prevention emphasizes controlling risk factors like diabetes, immunosuppression, and denture hygiene by ensuring proper cleaning and reducing sugar intake. Managing both conditions involves professional diagnosis, targeted treatments such as antifungal therapy for candidiasis and biopsy or removal for suspicious leukoplakia lesions, alongside ongoing oral health maintenance.
Prognosis and Long-term Follow-up
Leukoplakia carries a variable risk of malignant transformation, necessitating regular long-term follow-up with periodic biopsies to monitor dysplastic changes and prevent progression to oral squamous cell carcinoma. Oral candidiasis, often a secondary infection, typically resolves with antifungal treatment and has a favorable prognosis without long-term malignant potential. In contrast, leukoplakia demands continuous surveillance due to its premalignant nature and potential for recurrence or malignant transformation over time.
Leukoplakia, Oral candidiasis Infographic
 libterm.com
libterm.com